Key messages
- According to the reported data from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey, 8% of Aboriginal and Torres Strait Islander people living in non-remote areas reported seeing a doctor outside normal business hours in the previous 12 months.
- For Indigenous Australians, the Medicare data indicated that Medicare Benefits Schedule claims for after-hours services ranged from 147 claims per 1,000 population in Remote areas to 652 per 1,000 population in Major cities in 2017–18.
- Data from the 2017–18 Online Services Report showed that the main types of services provided by Indigenous primary health-care organisations during after-hours were transport (72% of organisations that provided some type of after-hours service), followed by treatment of injury (69%), diagnosis and treatment of infectious illness/diseases (61%), and social and emotional wellbeing/mental health/counselling services (57%).
- In the period July 2017 to June 2019, there were 1,124,770 emergency department presentations for Indigenous Australians (6.8% of all emergency department presentations), of which 58% (651,171 presentations) occurred after hours.
- Of all after-hours emergency department presentations for Indigenous Australians, 51% (332,462 of 651,171 presentations) were classified as semi-urgent or non-urgent.
Why is it important?
‘After-hours’ health care refers to services provided on Sundays, before 8 am and/or after 12 pm on a Saturday, or at any time other than 8 am to 6 pm on weekdays. An important component of comprehensive primary health care services is the capacity for patients to access services after hours. At the same time, many factors contribute to uptake of after-hours care, including perceptions of health care effectiveness, severity of illness, family requirements, convenience, location and the availability of in care services. The absence of after-hours primary health care may result in delays by patients to seek care and the importance of after-hours care for ongoing treatment should be recognised. After-hours care is also a practical strategy for improving continuity and coordination of care, often through flexible service delivery relative to patient needs. Technology plays a role in improving the operation of after-hours care and streamlining administrative processes, with strategies such as sharing of electronic patient records across settings in real time, use of telehealth and embedded use of case conferences between services.
It is often preferable for after-hours primary care to be provided by a patient’s usual general practitioner (GP), because the GP is more likely to know the patient’s condition and history and be able to provide an informed judgement about the treatment required. Many patients are provided with after-hours primary care services by their regular GP or at their usual health service through extended hours clinics, on-call arrangements, the provision of home visits, and cooperative arrangements that involve GPs from several practices participating in a shared roster system.
As this is not always possible, several of other after-hours primary care arrangements exist. These include medical deputising services (where GPs contract another service to provide after-hours services on their behalf), dedicated after-hours services (GP and/or nurse-led clinics that only open during the after-hours period) and telephone triage and advice services (which involve telephone-based nurses and/or GPs providing advice and directing people to the most appropriate point of care). Many patients also attend emergency departments during the after-hours period.
The Medicare Benefits Schedule (MBS) includes after-hours items that provide increased benefit rates to medical practitioners. Rates are highest for urgent after-hours consultations where practitioners are required to provide a home visit or return to the clinic specifically for that consultation.
Data findings
In the 2018–19 National Aboriginal and Torres Strait Islander Health Survey, 8% of Aboriginal and Torres Strait Islander people living in non-remote areas reported seeing a doctor outside normal business hours in the previous 12 months (Table D3.16.1).
According to 2017–18 Medicare data on MBS services claimed for after-hours care items, there were 312,886 after-hours services provided to Indigenous Australians, representing 2.5% of all after-hours MBS services provided. Note that these data may double-count after-hours care provided in selected emergency departments. After adjusting for differences in the age structure between the two populations, the rate of after-hours MBS services claimed for Indigenous Australians was 0.8 times that for non-Indigenous Australians (397 compared with 492 claims per 1,000 population) (Table D3.16.1).
For Indigenous Australians, MBS claims for after-hours services ranged from 147 per 1,000 population in Remote areas to 652 per 1,000 in Major cities (Figure 3.16.1).
Figure 3.16.1: Age-standardised rate of MBS services claimed for after-hours care, by Indigenous status and remoteness, 2017–18
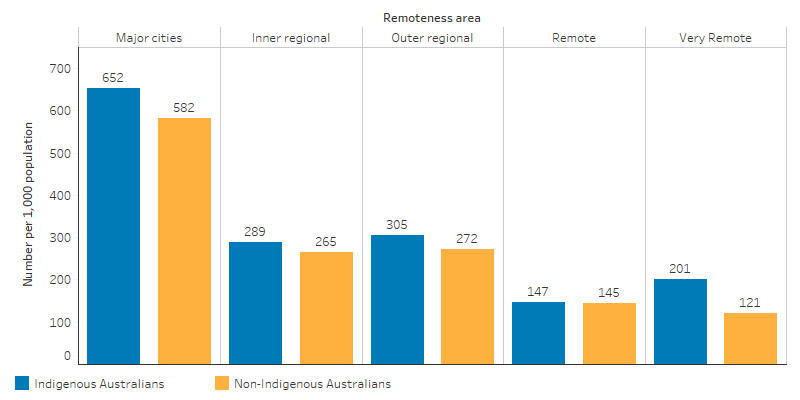
Source: Table D3.16.3. AIHW analysis of Medicare data.
By jurisdiction, rates varied from 165 per 1,000 in the Northern Territory to 661 per 1,000 in South Australia (Figure 3.16.2). Rates for after-hours MBS services claimed for Indigenous Australians were 1.7 times the rate for non-Indigenous Australians in Very remote areas. In the Northern Territory, the rate for Indigenous was only 34% as high for non-Indigenous (Table D3.16.3, Figure 3.16.1, Figure 3.16.2).
Figure 3.16.2: Age-standardised rate of MBS services claimed for after-hours care, by Indigenous status and jurisdiction, 2017–18
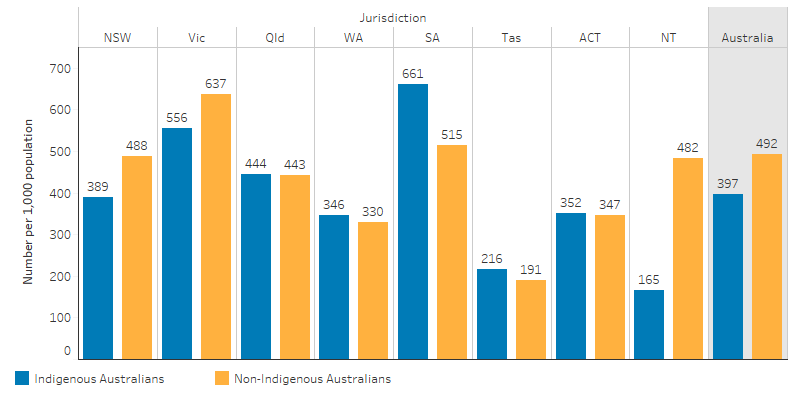
Source: Table D3.16.3. AIHW analysis of Medicare data.
The Bettering the Evaluation and Care of Health (2010–15) survey data estimated that 84% of general practitioner encounters for Indigenous patients were with practices that had after-hours care arrangements in place, compared with 96% for Other Australians (Table D3.16.4, Figure 3.16.3).
Figure 3.16.3: Rate of GP encounters, by whether the GP has after-hours arrangements in place, by Indigenous status of the patient, April 2010–March 2015
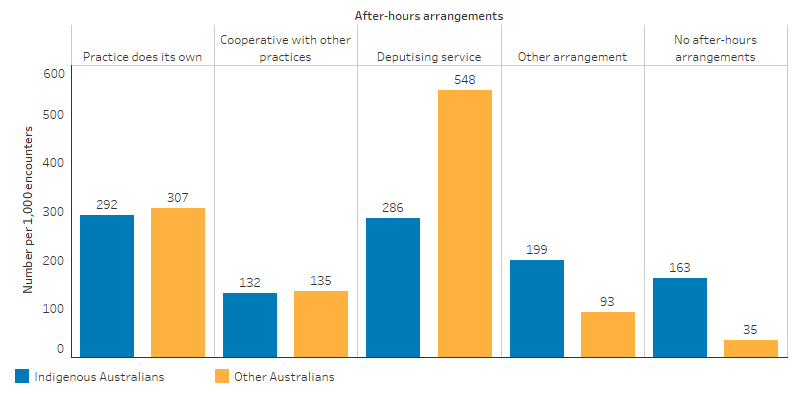
Source: Table D3.16.4. AIHW and Family Medicine Research Centre, University of Sydney analysis of BEACH data.
Data from the 2017–18 Online Services Report showed that 47% of Commonwealth-funded Indigenous primary health-care organisations provided after-hours services. The main types of services provided after hours were transport (72% of organisations that provided some type of after-hours service), followed by treatment of injury (69%), diagnosis and treatment of infectious illness/diseases (61%), and social and emotional wellbeing/mental health/counselling services (57%). Other after-hours services provided included: antenatal care (39%), care in police station/lock-up (37%), maternal and childcare (31%), diagnosis and treatment of chronic illness/disease (29%), substance use/drug and alcohol programs (24%), hospital inpatient/outpatient care (15%) and tobacco programs (8%) (Table D3.16.5).
Emergency department presentations
Data on services provided by emergency departments are limited to large public hospitals, mainly located in major cities. In these hospitals, in the period July 2017 to June 2019, there were 1,124,770 emergency department presentations by Indigenous Australians (6.8% of all emergency department presentations, excluding presentations where Indigenous status was unknown) (Table D3.16.6).
Between July 2017 and June 2019, about half (53%, 594,276) of emergency department presentations for Indigenous Australians were triaged as semi-urgent (needing to be seen within 60 minutes of presenting to an emergency department) or non-urgent (within 120 minutes). Of semi urgent and non-urgent presentations for Indigenous Australians, 72% occurred between 9am and 9pm, with a peak at 11am. A similar pattern in time of arrival was observed for non-Indigenous Australians, though the proportion of semi-urgent and non-urgent presentations that occurred between the hours of 4pm and 5am was slightly higher for Indigenous than non-Indigenous Australians (Table D3.16.7, Figure 3.16.4).
Figure 3.16.4: Emergency department presentations for triage categories 4 (semi-urgent) and 5 (non-urgent), by time of day and Indigenous status, July 2017–June 2019
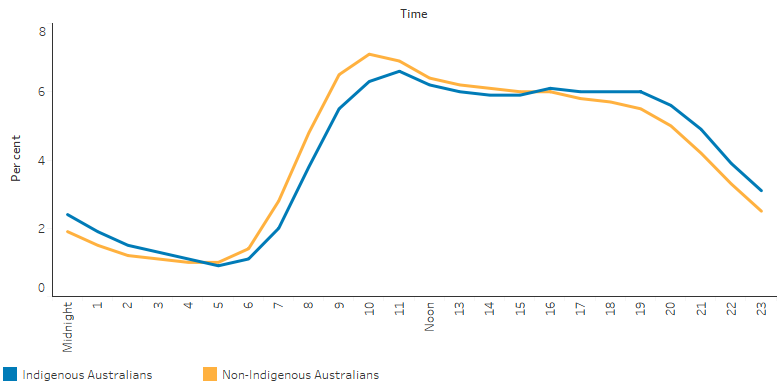
Source: Table D3.16.7. AIHW analysis of National Non-admitted Patient Emergency Department Care Database.
Emergency department presentations are considered to be after-hours if they occur on a Sunday, before 8am or from 12pm on a Saturday, or before 8am or from 6pm on a weekday.
Of all emergency department presentations for Indigenous Australians, 58% (651,171 presentations) occurred after hours – consisting of 355,988 after-hours presentations on a weekday (32% of all presentations), and 295,183 after-hours presentations on weekends (26%). Among after-hours emergency department presentations for Indigenous Australians, 51% were classified as semi-urgent or non-urgent (Table D3.16.8, Table 3.16-1) (for further definitions see measure 3.14 Access to services compared with need).
Table 3.16-1: Emergency department after-hours presentations, by Indigenous status, July 2017 to June 2019
|
All emergency department presentations |
Indigenous number |
Non-Indigenous number |
Indigenous % |
Non-Indigenous % |
|---|---|---|---|---|
|
On Sunday |
164,735 |
2,267,540 | 14.6 | 15.0 |
|
Before 8am or after 12pm on Saturday |
130,448 |
1,689,960 |
11.6 |
11.2 |
|
After-hours weekday (before 8am or from 6pm) |
355,988 |
4,418,332 | 31.6 | 29.2 |
|
Total after-hours |
651,171 | 8,375,832 | 57.9 | 55.4 |
|
Between 8am and 12pm on Saturday |
29,289 | 464,991 | 2.6 | 3.1 |
|
Between 8am and 6pm weekdays |
444,310 | 6,277,622 | 39.5 | 41.5 |
|
Not after-hours |
473,599 | 6,742,613 | 42.1 | 44.6 |
|
Total (a) |
1,124,770 | 15,118,445 | 100.0 |
100.0 |
|
Semi-urgent or non-urgent (triage category 4 and 5) emergency department presentations |
Indigenous number |
Non-Indigenous number |
Indigenous % |
Non-Indigenous % |
|---|---|---|---|---|
|
On Sunday |
90,136 | 1,135,049 |
15.2 |
15.7 |
|
Before 8am or after 12pm on Saturday |
67,978 | 801,649 | 11.4 | 11.1 |
|
After-hours weekday |
174,348 | 1,943,353 | 29.3 | 26.9 |
|
Total after-hours |
332,462 | 3,880,051 | 55.9 | 53.7 |
|
Between 8am and 12pm on Saturday |
18,005 | 259,181 | 3.0 | 3.6 |
|
Between 8am and 6pm weekdays |
243,809 | 3,087,896 | 41.0 | 42.7 |
|
Not after-hours |
261,814 | 3,347,077 | 44.1 | 46.3 |
|
Total (a) |
594,276 | 7,227,128 | 100.0 | 100.0 |
(a) Records are excluded where the patient's Indigenous status was unknown.
Note: These data are limited to large public hospitals mainly located in major cities.
Source: Tables D3.16.8, D3.16.9. AIHW analysis of National Non-admitted Patient Emergency Department Care Database.
For Indigenous Australians, the proportion of after-hours emergency presentations that were considered semi-urgent or non-urgent ranged across states and territories from 39% in Queensland (52,422 after-hours semi/non-urgent presentations) to 57% (131,623) in New South Wales (Table 3.16.10, Table 3.16.11).
Research and evaluation findings
Canuto and colleagues (2018) identified the perceived motivators, barriers and enablers of the utilisation of primary health care services among Indigenous males, and note the important role of after-hours care for service uptake (Canuto et al. 2018). The study explores patient experiences and suggestions to improve the uptake of services by Indigenous men in South Australia and Far North Queensland. Factors that motivated patients to use primary health care services included: patient judgements about ‘feeling sick’ and the requirement for action; the need for a specific service; personal importance of regular check-ups; and family encouragement. Barriers to the use of health care included long waiting times; inconvenient opening hours, lack of health knowledge; and culturally inappropriate staff or services. These factors are, in turn, important to the discovery and discussion of factors that could encourage the use of primary health care. Suggestions made by the study participants to improve service accessibility included: increasing opening hours; better proximity to work and home; and bringing services to patients that work full-time. Convenience was noted as a deciding factor for service uptake, often above perceived quality of service. Participants advocated the provision of after-hours health services.
De Witt and colleagues (2020) examined service improvement for Indigenous cancer patients in Queensland, including the importance of accessible and coordinated after-hours care (de Witt et al. 2020). Interviews were conducted with health professionals at several Aboriginal Community Controlled Health Services and one tertiary hospital. Results were analysed relative to the World Health Organization integrated people-centred health services framework that promotes health systems that are driven by continuity and coordination of care. A key driver of continuity and coordination of care is ‘flexible continuity’ (the ability to adjust care and treatment plans in response to patients changing individual needs across time). Factors that may improve the ‘flexible continuity’ of health systems include: flexible care delivery, such as telehealth; ‘Drop-in’ clinics; extension of primary health care clinic hours; longer patient consultations; consideration of individual patient needs when scheduling appointments; and availability of clinics outside of business hours to access allied health staff.
A review of after-hours primary health care in 2014 found significant variation in the arrangements for after-hours care across Australia, particularly between Remote and Non-remote areas and provided recommendations for future arrangements (Jackson 2014). The review found:
- unnecessarily complex processes for managing services
- benefits and drawbacks of competition between services
- a need for better triaging of care
- a lack of patient awareness of services available
- stakeholder concerns over the integration and continuity of care between regular sources of care and after-hours care.
The review found that better use of eHealth solutions would provide patients with tools to self-manage and enhance communication with regular care providers and improve continuity of care. There was strong interest among providers in returning after-hours care arrangements to a Practice Incentive Program payment.
Following this review, changes to arrangements relating to after-hours service provision were implemented on 1 July 2015, coinciding with the advent of Primary Health Networks (PHNs), which included:
- a PIP After-Hours Incentive payment available to eligible accredited general practices registered for the PIP
- funding to PHNs to support locally tailored after-hours services
- the new after-hours GP advice and support line to better support all Australians who do not have access to face-to-face GP services in the after-hours period.
Implications
Nationally, Indigenous Australians have a lower rate of MBS after-hours services claimed than non-Indigenous Australians (rate ratio of 0.8). However, this masks some variation by jurisdictions and remoteness. Rates were particularly low in Remote and Very remote areas for both Indigenous and non-Indigenous Australians and the largest gap was in the Northern Territory (rate ratio of 0.3).
Indigenous Australians accounted for 7% of the total after-hours presentations to emergency departments with over half of these being semi-urgent or non-urgent.
A better understanding is required of the needs of Indigenous Australians for health services after-hours, and the best ways of providing coverage.
The PIP After-Hours Incentive is designed to provide a nationally consistent model for access to after-hours primary health care for the majority of Australia. Recognising that the PIP after-hours incentive is not a one-size-fits-all solution, PHNs are being funded to address gaps in after-hours service provision, including where there is an unmet need. PHNs will focus on access to care for ‘at-risk’ or vulnerable populations (such as Indigenous Australians) and improving service integration, particularly where gaps exist due to a lack of access to general practices registered for the PIP After-Hours Incentive.
Evaluation of these changes to after-hours service provision is needed to assess the effectiveness of meeting the needs of vulnerable populations such as Indigenous Australians. Existing barriers to accessing primary health care will be factors in accessing after-hours care. The cultural competency of service providers, particularly if these are not the usual care givers, will be an important factor in ensuring appropriate care.
The policy context is at Policies and strategies.
References
- Canuto K, Wittert G, Harfield S & Brown A 2018. “I feel more comfortable speaking to a male”: Aboriginal and Torres Strait Islander men’s discourse on utilizing primary health care services. International Journal for Equity in Health 17:185.
- de Witt A, Matthews V, Bailie R, Garvey G, Valery PC, Adams J et al. 2020. Communication, Collaboration and Care Coordination: The Three-Point Guide to Cancer Care Provision for Aboriginal and Torres Strait Islander Australians. International Journal of Integrated Care (IJIC) 20:1-16.
- Jackson C 2014. Review of after hours primary health care. (ed., Health AGDo). Australian Government Department of Health.

