Key messages
- In 2018–19, 58% of Aboriginal and Torres Strait Islander children aged under 15 had a dental consultation in the last 12 months based on survey data (with adults responding on behalf of the children), while 23% had never attended a dental practice
- An estimated 6% of Indigenous Australians aged 15 and over in 2018–19 had complete tooth loss and 45% had lost at least one tooth (excluding wisdom teeth), based on self-reported survey data.
- In 2018–19, an estimated 19% of Indigenous Australians did not go to a dentist when they needed to in the previous 12 months (based on self-reported survey data). The reasons reported include cost (42%); being too busy (24%); disliked service or professional or felt embarrassed or afraid (22%); or waiting time too long or an appointment not available at the time required (15%).
- Between July 2017 and June 2019, Indigenous children aged 0–4 were hospitalised for dental conditions at 1.6 times the rate of non-Indigenous children; those aged 5–14 were hospitalised at 1.3 times the rate.
- Among Indigenous Australians, children aged 5–9 had the highest rate of hospitalisation for dental conditions involving general anaesthesia (12 per 1,000), followed by those aged 0–4 (7.4 per 1,000).
Why is it important?
Oral health refers to the health of tissues of the mouth: muscle, bone, teeth and gums. The two most frequently occurring oral diseases are tooth decay (termed ‘caries’) and gum (periodontal) disease. If not treated in a timely manner, these can cause discomfort and tooth loss, impacting a person's ability to eat, speak, and socialise without discomfort or embarrassment (Williams et al. 2011). Oral diseases can intensify other chronic diseases (Jamieson et al. 2010a) and have been found to be associated with cardiovascular diseases (Ylöstalo et al. 2006), diabetes (Taylor & Borgnakke 2008), stroke (Joshipura et al. 2003) and pre-term low birthweight (Roberts-Thomson et al. 2008; Williams et al. 2011; Xiong et al. 2006).
Aboriginal and Torres Strait Islander children and adults have much higher rates of dental disease than their non-Indigenous counterparts across Australia, which can be largely attributed to the social determinants of health, such as poverty, racism and the consequences of colonialism (Australian Medical Association 2019). Indigenous Australians are more likely than non-Indigenous Australians to have multiple caries, have lost all their teeth, and/or to have gum disease (Jamieson et al. 2010b) and also less likely to receive the dental care that they need (Jamieson et al. 2010a; Kruger & Tennant 2015; Slade et al. 2007).
Tooth decay can be largely prevented by diet (for example reducing intake of processed sugary foods/drinks), fluoridation of water supplies (Lalloo et al. 2015), appropriate use of fluoridated toothpaste, good oral hygiene and regular dental check-ups. The same risk factors apply to periodontal diseases as well as smoking, diabetes, stress, and substance use (particularly inhalant use). Lower levels of education and income and sub-standard living conditions are associated with oral diseases (Lalloo et al. 2016). In addition to oral hygiene and dental care, tooth loss is associated with increased age and accidents and injuries (Jamieson et al. 2010a; Williams et al. 2011).
The National Aboriginal and Torres Strait Islander Health Plan 2021-2031 (the Health Plan), released in December 2021, provides a strong overarching policy framework for Aboriginal and Torres Strait Islander health and wellbeing. The Health Plan was developed in genuine partnership with Aboriginal and Torres Strait Islander leaders and is the first national health document to address the health targets and priority reforms of the National Agreement on Closing the Gap (the National Agreement).
‘Priority Five’ focuses on early intervention approaches that are accessible to Indigenous Australians and provide timely, high quality, effective, culturally safe and responsive care. One objective specifically addresses oral health:
- Objective 5.2. Deliver activities to improve oral health, particularly for children
The Health Plan is discussed further in the Implications section of this measure.
Burden of disease
In 2018, oral disorders accounted for 2.1% (4,952 out of 239,893 total DALY) of the total disease burden for Indigenous Australians, and 3.9% (4,917 out of 126,447 total YLD) of the non-fatal burden (years lived with disability). Indigenous males experienced slightly more of the total burden due to oral disorders than Indigenous females (53% compared with 47%, respectively).
Dental caries was the leading cause of oral disease burden among Indigenous Australians, accounting for almost two-thirds (63%; 3,117 out of 4,952 total DALY due to oral disorders) of the burden due to oral disorders. This was followed by periodontal disease (22%; 1,081 DALY) and severe tooth loss (15%; 741 DALY).
Dental caries accounted for almost all (99.7%; 505 out of 507 total DALY due to oral disorders) of the oral disorders burden for Indigenous Australians aged between 5–14 years, but generally had a decreasing contribution with age thereafter. For Indigenous Australians over the age of 65, severe tooth loss was the leading cause of burden (48%; 315 out of 651 total DALY due to oral disorders), followed by dental caries (27%; 179 DALY) and periodontal disease (25%; 163 DALY). Between 2003 and 2018, for Indigenous Australians, the total burden attributable to oral disorders increased by 17% (based on age-standardised rates). This was predominantly driven by an increase in the non-fatal burden (AIHW 2022a, 2022b).
Data findings
Oral health based on self-reported data
Data on oral health and dental consultations are available from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey, based on self-report (for children under 15, an adult was asked to respond on their behalf).
Based on these data, in 2018–19, 81% of Indigenous Australians brushed their teeth daily and 45% brushed their teeth twice a day. An estimated 50% of Indigenous Australians had seen a dentist in the last 12 months and 12% had never seen a health professional about teeth.
Of Indigenous Australians who had previously seen a dentist, 38% had last visited a private dental clinic, 28% a government dental clinic, 12% a school dental clinic, and 18% a dentist at an Aboriginal Medical Service. Among Indigenous Australians living in non-remote areas who had last received non-urgent dental treatment at a public dental service, almost half (49%) waited less than a week (including did not wait at all). Conversely, 13% waited 3 months or more. (Table D1.11.11).
An estimated 19% of Indigenous Australians did not go to a dentist when they needed to in the previous 12 months, based data from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey. Reasons included: cost (42%), too busy (24%), disliking service or professional, or feeling embarrassed or afraid (22%) and waiting time too long or not available at time required (15%) (Table D3.08.3, Figure 1.11.1).
Figure 1.11.1: Indigenous Australians who needed to go to a dentist in the last 12 months but did not, by reason, 2018–19
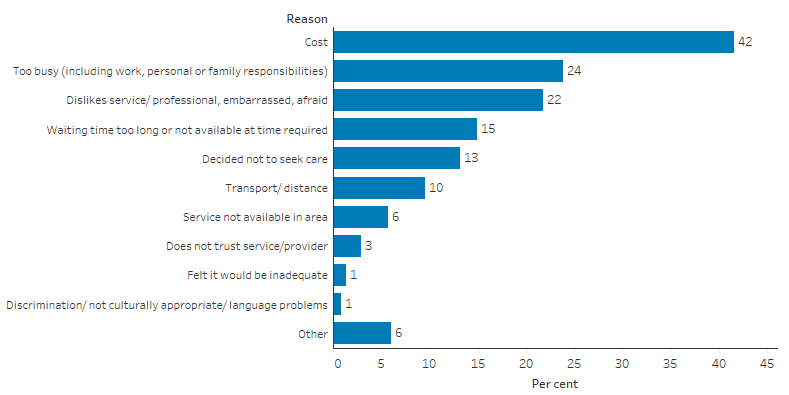
Source: Table D3.08.3. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
In 2018–19, an estimated 82% of Indigenous children aged 0–14 brushed their teeth daily, 58% had their last appointment within the previous 12 months, and 23% had never seen a dentist.
Based on the 2018–19 survey, of around 183,000 Indigenous children aged 0–14 who had seen a dentist, 30% had attended a school dental clinic for their most recent consultation, 28% attended a private clinic (including specialists), 24% attended a government dental clinic and 14% attended a dentist at an Aboriginal Medical Service. Of around 29,400 Indigenous children living in remote areas who had seen a dentist (Remote and Very remote areas combined), 38% went to a school dental clinic, compared with 28% of those in non-remote areas (Major cities, Inner and Outer regional areas combined) (Table D1.11.29, Figure 1.11.2).
Figure 1.11.2: Place of last dental consultation among Indigenous children aged 0–14 who had attended a dental practice, by remoteness, 2018–19
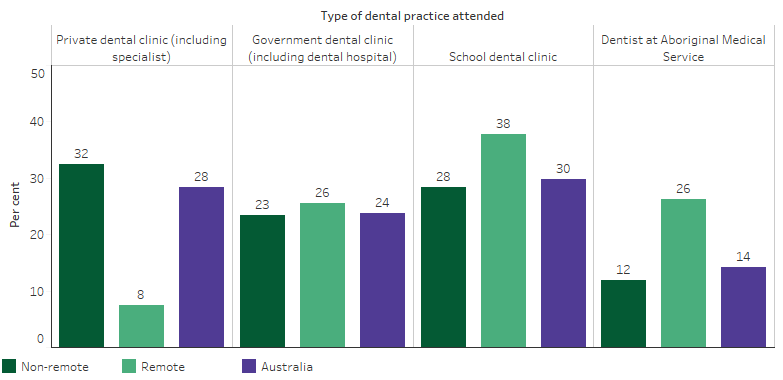
Note: Denominator for the percentages is the number of children aged 15 and over who had attended a dental practice (in non-remote areas, remote areas, or Australia, as applicable).
Source: Table D1.11.29. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
In 2018–19, an estimated 3% of Indigenous children aged 0–14 needed to go to the dentist in the past 12 months but did not. The most common reasons parents attributed this to were cost (32%); disliked service or professional or felt embarrassed or afraid (17%); too busy (16%); or waiting time or an appointment not available at the time required (13%) (Table D3.08.3).
Based on data from the 2014–15 National Aboriginal and Torres Strait Islander Social Survey, 28% of Indigenous children aged under 15 had teeth or gum problems in 2014–15 (Table D1.11.1). The most common types of problems reported were cavities or dental decay (12%), fillings due to dental decay (11%), needing braces/plate/retainer (6%) and having teeth pulled out due to dental decay (5%) (Table D1.11.3, Figure 1.11.3).
Figure 1.11.3: Proportion of Indigenous children aged 0–14 with reported teeth or gum problems, by type of dental or gum problem, 2014–15
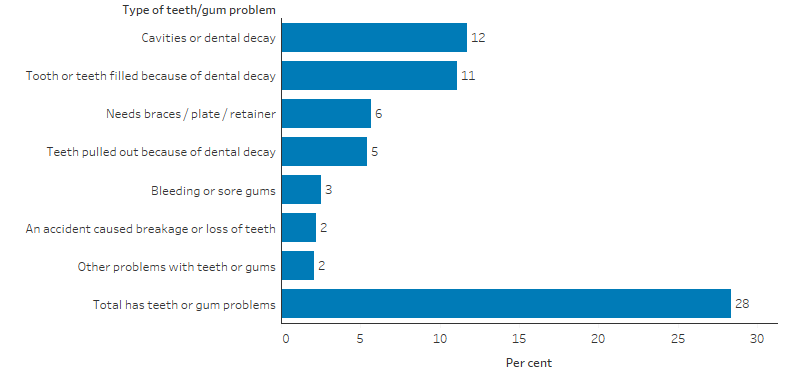
Source: D1.11.3. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Social Survey 2014–15.
Based on survey estimates, of around 63,400 Indigenous children with teeth or gum problems, 56% had experienced the problem for at least 12 months. This was more common for Indigenous children living in non-remote areas (58% of those with teeth or gum problems) compared with remote areas (45%) (Table D1.11.5). Of around 63,000 Indigenous children with teeth or gum problems, 29% of had their last dental check less than 3 months ago and 8% had never been to a dentist (Table D1.11.6).
Across age groups, the proportion of Indigenous children with reported teeth or gum problems was 39% for those aged 10–14 (an estimated 28,900 children), 33% for those aged 5–9 (26,800 children), and 11% for those aged 0–4 (7,400 children) (Table D1.11.4).
Child Dental Benefits Schedule services
In 2015, 45,396 Indigenous children received dental services under the Child Dental Benefits Schedule, representing 20% of those eligible for these services. In comparison, 35% of eligible non-Indigenous children had received these services (Table D1.11.26).
Child dental health services in the Northern Territory
Between August 2007 and December 2018, 37,005 dental services were provided to 13,786 Indigenous children under the National Partnership Agreement on Northern Territory Remote Aboriginal Investment (NTRAI). Over this period, 86% of Indigenous children who had a dental service had two or more dental checks (Table D1.11.22). Over half (51%) of Indigenous children who received a dental service were aged 6–11 (Table D1.11.23).
Between August 2007 and June 2012, 7,403 Indigenous children received dental services under the Child Health Check Initiative Program and 46% of those children were treated for at least one dental problem. Thirty-eight per cent of Indigenous children who received dental services under the program were treated for untreated tooth decay (Table D1.11.25).
The Stronger Futures in the Northern Territory (SFNT) funding agreement began in July 2012 and continues to provide funding through the Northern Territory Remote Aboriginal Investment (NTRAI Extension 2022-24. The Health Implementation Plan under NTRAI supports hearing and oral health services to children aged under 16 in remote and very remote locations in the Northern Territory.
Between July 2012 and December 2018, 13,143 children received 25,419 clinical services. The numbers fluctuated over time but were lower in 2018 than in 2016 or 2017. The proportion of dental service recipients with tooth decay decreased for most age groups between March 2009 and December 2018. The largest decrease was for Indigenous children aged 1–3 years combined (from 73% to 41%), followed by those aged 12 years (from 81% to 63%) (AIHW 2019).
Tooth loss
In the 2018–19 National Aboriginal and Torres Strait Islander Health Survey, data was collected on tooth loss, based on self-report. Based on this, an estimated 6% of Indigenous Australians aged 15 and over were had complete tooth loss, and a further 45% had lost at least one tooth (excluding wisdom teeth) (Table D1.11.7, Figure 1.11.4).
Figure 1.11.4: Status of tooth loss of Indigenous persons aged 15 and over, by age, 2018–19
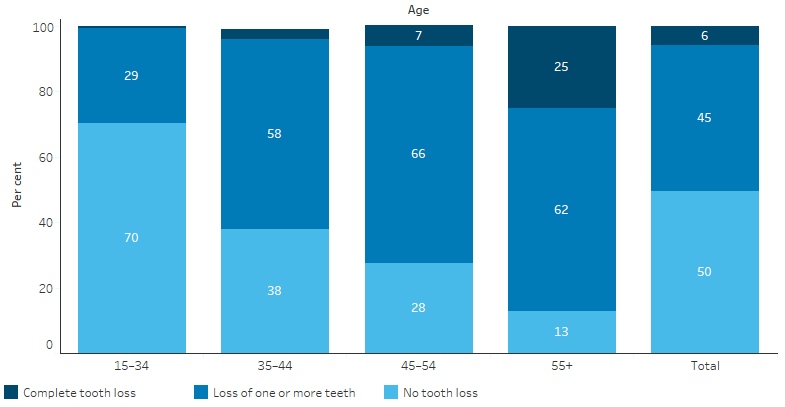
Source: Table D1.11.7. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
In 2018–19, by age group, rates of complete tooth loss were highest for Indigenous Australians aged 55 and over, with one-quarter (25%) having complete tooth lost. The proportion of Indigenous Australians aged 55 and over with complete tooth loss was higher in non-remote than remote areas – 26% (18,000 people) in non-remote areas, compared with 22% (3,300 people) in remote areas (Table D1.11.10).
The proportion of Indigenous Australians with complete tooth loss was higher for those with: three or more long term health conditions (8.6 times those with no conditions); Year 9 or below as the highest year of schooling (8 times those with Year 12); the lowest income (4.9 times those with the highest income); heart or cardiovascular (circulatory) problems (4.9 times those without heart/cardiovascular problems); and reported diabetes or high blood sugar levels (4 times those without diabetes or HSL) (Table D1.11.8, Table D1.11.9).
Hospitalisations for dental problems
Between July 2017 and June 2019, there were about 4,100 hospitalisations among Indigenous Australians due to dental caries; loss of teeth due to accident, extraction or local periodontal disease; or dental examination. This a rate of 2.5 hospitalisations per 1,000 population and accounting for 0.7% of all hospitalisations of Indigenous Australians (excluding dialysis) (Table D1.02.1, Table D1.11.21). Indigenous children aged 0–4 and 5–14 had the highest rate of hospitalisation, at 5.8 and 5.9 per 1,000 population respectively, with rates ranging between 0.4 and 0.9 per 1,000 population in older age groups.
Indigenous children aged 0–4 were hospitalised for dental conditions at 1.6 times the rate of non-Indigenous children and those aged 5–14 were hospitalised at 1.3 times the rate. Conversely, among people aged 55–64 and 65 and over, the rate of hospitalisation due to dental problems was lower for Indigenous Australians than for non-Indigenous Australians (Table D1.11.21, Figure 1.11.5).
Figure 1.11.5: Age-specific hospitalisation rates for a principal diagnosis of dental problems, by Indigenous status and age, Australia, July 2017 to June 2019
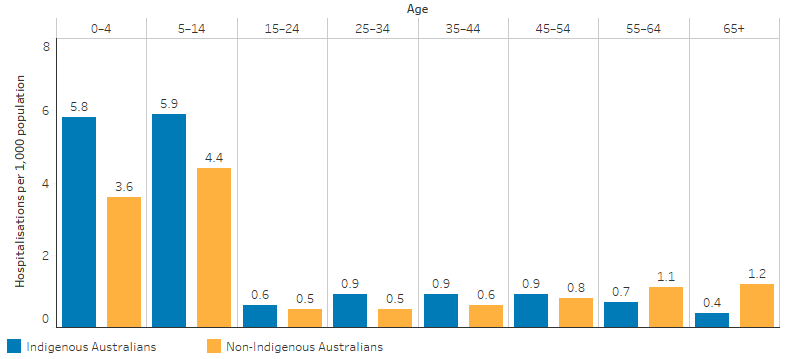
Note: Principal diagnosis of dental problems includes dental caries; loss of teeth due to accident, extraction or local periodontal disease; and dental examination.
Source: Table D1.11.21. AIHW analysis of National Hospital Morbidity Database.
Dental care under general anaesthetic carries an additional risk and is resource intensive. Among Indigenous Australians, there were 8,401 hospitalisations for dental procedures that involved general anaesthesia between July 2017 and June 2019 – a rate of 5.1 per 1,000 population.
The highest rates were for Indigenous children aged 5–9 (12 per 1,000) followed by those aged 0–4 (7.4 per 1,000). Rates of hospitalisation for dental procedures involving general anaesthesia were lower for Indigenous Australians than non-Indigenous Australians across most age groups. The exception was for those aged between 25–34 where the rates were similar (3.0 compared with 2.8 per 1,000 for Indigenous and non-Indigenous Australians, respectively) and those aged 35–44 (both 2.5 per 1,000) (Table D1.11.28).
Data on hospitalisation due to periodontal disease indicates that, overall, the rate was similar for Indigenous and non-Indigenous Australians (Table D1.11.31). However, this varied by age group. In every age group except those aged 65 and over, the rate of hospitalisation due to periodontal disease was higher for Indigenous than non-Indigenous Australians. Indigenous Australians aged 25–34 were 3.8 times as likely to be hospitalised for periodontal disease compared with non-Indigenous Australians (Table D1.11.31).
Child Dental Health Survey
In the 2010 Child Dental Health Survey, the average number of decayed, missing or filled deciduous teeth (baby teeth) among Indigenous children aged 5–10 was 1.7 times the number for non-Indigenous children (3.8 and 2.2, respectively) in the six jurisdictions combined with data of adequate quality (Queensland, Western Australia, South Australia, Tasmania, the Australian Capital Territory and the Northern Territory) (Table D1.11.13). Indigenous children aged 5–10 were less likely to have no decayed, missing or filled deciduous teeth (24%) than non-Indigenous children (45%) (Table D1.11.14, Figure 1.11.6).
Figure 1.11.6: Proportion of children aged 5–10 with no decayed, missing or filled deciduous teeth (DMFT = 0), by age and Indigenous status, 2010
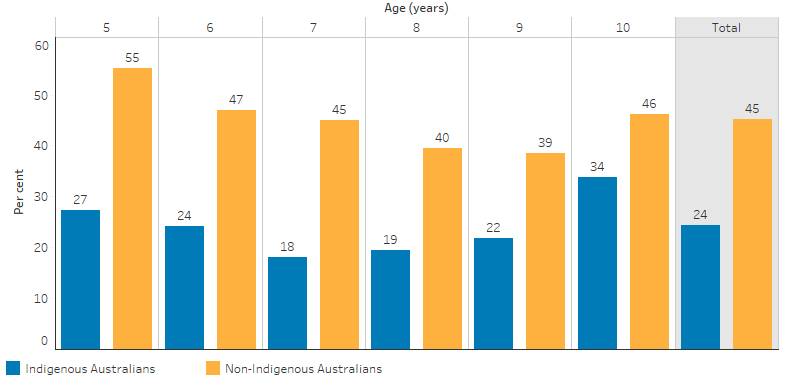
Source: Table D1.11.14. AIHW analysis of Child Dental Health Survey 2010.
By age 14–15, Indigenous children had on average, twice as many decayed teeth, 2.8 times the number of missing teeth and 1.4 times the number of filled teeth than non-Indigenous children (Table D1.11.15). For those aged 6–15, 48% of Indigenous children had no decayed, missing or filled permanent teeth compared with 63% of non-Indigenous children (Table D1.11.16, Figure 1.11.7).
Figure 1.11.7: Proportion of children aged 6–15 with no decayed, missing or filled permanent teeth (DMFT = 0), by age and Indigenous status, 2010
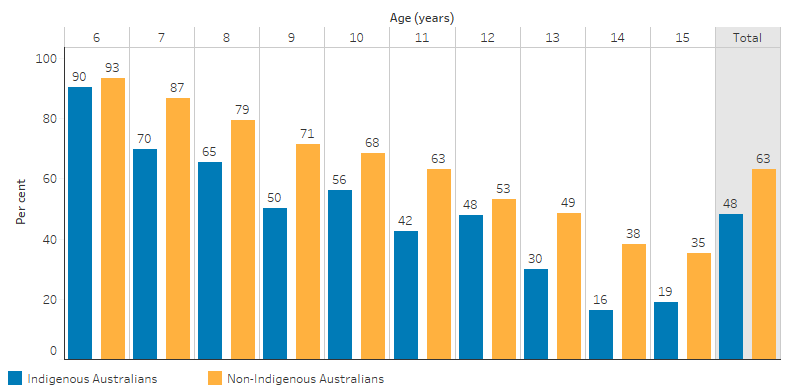
Source: Table D1.11.16. AIHW analysis of Child Dental Health Survey 2010.
Research and evaluation findings
Poor oral health is strongly associated with low socioeconomic status. Research has shown that adults who are socially disadvantaged or on a low income have more than double the rate of poor oral health than those on higher incomes, including higher rates of untreated decay (Brennan et al. 2019).
Western dental approaches (for example fluoride varnish), while clinically efficacious may not be enough to lead to lasting dental improvement in Indigenous Australian children, where other determinants such as socioeconomic status, access to services, and cultural and environmental factors act as barriers to oral health (Patel et al. 2017; Smith et al. 2007; Williams et al. 2011). Community-based interventions for oral health care should build on community strengths and harness local Indigenous Health Workers to work with families and communities in oral health promotion (Slade et al. 2011).
An effective program in Port Augusta, South Australia, highlighted the challenges in achieving this mix of community engagement, health promotion and provision of dental services. The program also faced a number of hurdles with patient attendance, including difficulties with transport, and a lack of understanding of the importance of dental health among Indigenous Australian families (Parker et al. 2012).
In South Australia, the Aboriginal Health Program introduced in 2005 saw an increase of Indigenous Australians accessing mainstream dental care from 60 to 4,800 people by 2014–15. The key strategies of the program include: ensuring Indigenous adults are referred to dental services for free general and emergency dental care with no waiting lists; increasing the number of Indigenous teenagers accessing dental care; ensuring Indigenous children can access dental care from a variety of pathways; working with health professionals and pregnant women to increase their oral health knowledge; and to develop a range of oral health resources for Indigenous Australians (The University of Adelaide 2020).
Development and implementation of evidence based oral health promotion and prevention programs is fundamental to effective provision of appropriate services to meet population oral health needs. Improving the evidence base for oral health promotion programs for Indigenous Australians is necessary (COAG Health Council 2015).
Patel et al. (2017) published a review of oral health interventions for Indigenous Australian communities (Patel et al. 2017). The review found oral health interventions should not just be community-based but also community-driven with a shared understanding of outcomes, and mutually reinforcing and coordinated activities including using the skills of local staff and building capacity in oral health promotion. However, the impact of social determinants beyond the delivery of oral health services will continue to limit the effect of oral health interventions on Indigenous health outcomes, and contribute to the disparity between Indigenous and non-Indigenous Australians.
Gwynn et al. (2020) published a review of international studies and evaluations of community based oral health interventions targeting indigenous adolescents and found a shortage of good quality evaluations (Gwynn et al. 2020). Studies lacked strong indigenous community engagement, governance or leadership. The review recommended that this must be included in community based oral health interventions and research.
An international systematic review of oral health programs for indigenous communities found that programs should include extensive community involvement before, during and after implementation to enhance ownership and participation. Programs should incorporate advocacy and community development, utilise evidence-based interventions which include traditional models of health, secure funding stability, include strategies to ensure staff retention, and develop strategies that target the broader determinants of oral health (Tsai et al. 2017).
Implications
Available data indicate that dental health is worse for Indigenous Australians than for non-Indigenous Australians, particularly children. Barriers to good oral health include cost of services (see measure 3.14 Access to services compared to need) and healthy diets on limited budgets (see measure 2.19 Dietary behaviours). Further barriers include attending services for pain not prevention, insufficient education about oral health and preventing disease, public dental services not meeting demand, lack of fluoridation in some water supplies, and cultural competency issues with some service providers (see measure 3.08 Cultural competency ) (Durey et al. 2016; Dyson et al. 2014; Johnson et al. 2014).
The National Oral Health Plan 2015–2024 aims to improve the oral health status of Australians by reducing the incidence, prevalence and effects of oral disease and to also reduce inequalities in oral health status across the Australian population. It identifies Aboriginal and Torres Strait Islander people as a priority population. Key strategies for improving oral health outcomes and reducing the impact of poor oral health for Indigenous Australians include:
- Increase community engagement in the planning and delivery of oral health services
- Promote the incorporation of cultural competency across services that incorporate training, education and assessment, clinical management protocols and guidelines
- Develop integrated models of care that incorporate oral health education, prevention and screening with other primary care services
- Increase the representation and engagement of Aboriginal and Torres Strait Islander people in the oral health workforce
- Expand existing primary health practice incentives and funding adjustments for oral health services for Aboriginal and Torres Strait Islander people.
Dental health workforce shortages in remote areas need to be addressed with creative solutions beyond financial incentives to improve workforce retention. Stronger representation of Indigenous Australians in the dental health workforce will likely be highly valued by Indigenous patients, and improve the cultural safety of services and hospitals. Regulatory hurdles that affect some dental services (such as fluoride varnish) need to be overcome to improve the flexibility and delivery of effective dental care (Australian Medical Association 2019).
A significant body of work over the past two decades has sought to raise awareness and embed concepts of cultural respect in the Australian health system which are fundamental to improving access to quality and effective health care and improve health outcomes for Indigenous Australians. There has been a longstanding commitment by Australian governments to enable this. The Cultural Respect Framework 2016–2026 plays a key role in reaffirming this commitment and provides a nationally consistent approach, although it does not explicitly address oral health the broad domains that underpin culturally accessible, responsive and safe health service delivery are also applicable. The Aboriginal and Torres Strait Islander Health Performance Framework plays a role in monitoring this commitment across several measures (see measure 3.08 Cultural competency). Monitoring is also supported by the Cultural safety in health care for Indigenous Australians: monitoring framework which covers three domains: how health-care services are provided, Indigenous patients’ experience of health care, and measures regarding access to health care (AIHW 2022c). The 2022 Cultural safety report showed that a commitment to achieving culturally safe health care by Indigenous-specific health care organisations was 95% in 2017-18, an increase from 86% in 2012-13, while noting the lack of data available for reporting on the policies and practices of mainstream health services (AIHW 2022c).
The data also illustrates the importance of school dental programs for many Indigenous Australian children, particularly those living in remote areas. Schools are common settings for oral health interventions internationally as an opportunity for targeting student dental needs. However, they may be underutilised by Indigenous Australian children (Parker et al. 2012). This could mean mainstream school dental services lack cultural safety, but may be filling a service gap in the absence of a more suitable alternative, such as a culturally friendly children’s dental service incorporated into an Aboriginal Community Controlled Health Service.
School-based interventions may crowd out opportunities to deliver oral health promotion to families. Evidence suggests there is a lack of community understanding about the importance of oral health. This understanding could be built through community-driven programs working with dental care providers and with mutually reinforcing and coordinated activities that involve families. However, barriers to sustainable oral health improvements will remain until the broader social determinants and inequities affecting Indigenous Australians are addressed.
The Health Plan is the overarching policy framework to drive progress against the National Agreement health targets and priority reforms. The Health Plan was developed in genuine partnership with Aboriginal and Torres Strait Islander leaders. Implementation of the Health Plan aims to drive structural reform towards models of care that are prevention and early intervention focused, with greater integration of care systems and pathways across primary, secondary and tertiary care. It also emphasises the need for mainstream services to address racism and provide culturally safe and responsive care, and be accountable to Aboriginal and Torres Strait Islander people and communities.
The Health Plan suggests that efforts should be targeted at providing strengths based, culturally safe and holistic, affordable services to ensure early intervention across the life course, particularly in children as preventive care can help avoid oral disease later in life. The Health Plan’s oral health objective calls to expand access and funding for essential dental services and to drive uptake of dental health services and benefits, including the Child Dental Benefits Schedule which provides limited dental cover for eligible children aged 0-17. Partnering with communities to design and deliver these oral health programs is vital because it will maximise the chances of success (Dimitropoulos et al. 2020) and support the multifaceted approach to oral health services and education needed to reach children early (Butten et al. 2019).
Prevalence estimates for oral health conditions for Indigenous Australians are based on incomplete or out-of-date surveys—further data development is a priority for this performance measure.
A more coordinated and consistent approach to research and evaluation will provide the basis for continuous improvement of oral health services and systems.
The Policy Context is at Policies and Strategies.
References
- AIHW (Australian Institute of Health and Welfare) 2019. Northern Territory Remote Aboriginal Investment: Oral Health Program July 2012 to December 2018. Canberra: AIHW.
- AIHW 2022a. Australian Burden of Disease Study: Impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018. Canberra: AIHW.
- AIHW 2022b. Australian Burden of Disease Study 2018: Interactive data on risk factor burden among Aboriginal and Torres Strait Islander people. Canberra: AIHW. Viewed May 2022.
- AIHW 2022c. Cultural safety in health care for Indigenous Australians: monitoring framework. Canberra: AIHW. Viewed October 2022.
- Australian Medical Association 2019. 2019 AMA Report card on Indigenous health. No more decay: addressing the oral health needs of Aboriginal and Torres Strait Islander Australians.: Australian Medical Association.
- Brennan DS, Spencer AJ & Roberts-Thomson KF 2019. Socioeconomic and psychosocial associations with oral health impact and general health. Community Dentistry and Oral Epidemiology 47:32-9.
- Butten K, Johnson N, Hall K, Toombs M, King N & O'Grady KA 2019. Impact of oral health on Australian urban Aboriginal and Torres Strait Islander families: a qualitative study. International Journal for Equity in Health 18:1-10.
- COAG Health Council 2015. Healthy Mouths, Healthy Lives: Australia’s National Oral Health Plan 2015–2024. South Australian Dental Service Adelaide (AUST).
- Dimitropoulos Y, Holden A, Gwynne K, Do L & Sohn W 2020. Outcomes of a co-designed, community-led oral health promotion program for Aboriginal children in rural and remote communities in New South Wales, Australia. Community dental health 29:132-7.
- Durey A, McAullay D, Gibson B & Slack-Smith L 2016. Aboriginal Health Worker perceptions of oral health: a qualitative study in Perth, Western Australia. International Journal for Equity in Health 15:4.
- Dyson K, Kruger E & Tennant M 2014. A decade of experience evolving visiting dental services in partnership with rural remote Aboriginal communities. Australian Dental Journal 59:187-92.
- Gwynn J, Skinner J, Dimitropoulos Y, Masoe A, Rambaldini B, Christie V et al. 2020. Community based programs to improve the oral health of Australian Indigenous adolescents: a systematic review and recommendations to guide future strategies. BMC health services research 20:1-14.
- Jamieson LM, Roberts-Thomson KF & Sayers SM 2010a. Risk indicators for severe impaired oral health among indigenous Australian young adults. BMC Oral Health 10:1.
- Jamieson LM, Sayers S & Roberts-Thomson KF 2010b. Clinical oral health outcomes in young Australian Aboriginal adults compared with national-level counterparts. The Medical Journal of Australia 192:558-61.
- Johnson NW, Lalloo R, Kroon J, Fernando S & Tut O 2014. Effectiveness of water fluoridation in caries reduction in a remote Indigenous community in Far North Queensland. Australian Dental Journal 59:366-71.
- Joshipura KJ, Hung H-C, Rimm EB, Willett WC & Ascherio A 2003. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke 34:47-52.
- Kruger E & Tennant M 2015. Potentially preventable hospital separations related to oral health: a 10-year analysis. Australian Dental Journal 60:205-11.
- Lalloo R, Jamieson LM, Ha D, Ellershaw A & Luzzi L 2015. Does fluoride in the water close the dental caries gap between Indigenous and non-Indigenous children? Australian Dental Journal 60:390-6.
- Lalloo R, Jamieson LM, Ha D & Luzzi L 2016. Inequalities in Tooth Decay in Australian Children by Neighbourhood Characteristics and Indigenous Status. Journal of Health Care for the Poor and Underserved 27:161-77.
- Parker E, Misan G, Shearer M, Richards L, Russell A, Mills H et al. 2012. Planning, implementing, and evaluating a program to address the oral health needs of Aboriginal children in Port Augusta, Australia. International journal of pediatrics 2012.
- Patel J, Durey A, Hearn L & Slack‐Smith L 2017. Oral health interventions in Australian Aboriginal communities: a review of the literature. Australian Dental Journal 62:283-94.
- Roberts-Thomson KF, Spencer AJ & Jamieson L 2008. Oral health of Aboriginal and Torres Strait Islander Australians. The Medical Journal of Australia 188:592-3.
- Slade GD, Bailie RS, Roberts‐Thomson K, Leach AJ, Raye I, Endean C et al. 2011. Effect of health promotion and fluoride varnish on dental caries among Australian Aboriginal children: results from a community‐randomized controlled trial. Community Dentistry and Oral Epidemiology 39:29-43.
- Slade GD, Spencer A & Roberts-Thomson KF 2007. Australia's Dental Generations: The National Survey of Adult Oral Health, 2004-06. Cat. no. DEN 165. Canberra: AIHW.
- Smith K, Kruger E, Dyson K & Tennant M 2007. Oral health in rural and remote Western Australian Indigenous communities: A two‐year retrospective analysis of 999 people. International Dental Journal 57:93-9.
- Taylor GW & Borgnakke W 2008. Periodontal disease: associations with diabetes, glycemic control and complications. Oral diseases 14:191-203.
- The University of Adelaide 2020. Aboriginal Oral Health Program - SA Dental Service. Viewed 02/09/2020.
- Tsai C, Blinkhorn A & Irving M 2017. Oral Health Programmes in Indigenous Communities Worldwide-Lessons learned from the field: A qualitative systematic review. Community Dentistry Oral Epidemiology 45:389-97.
- Williams S, Jamieson L, MacRae A & Gray C 2011. Review of Indigenous oral health. Australian Indigenous HealthInfoNet No. 7.
- Xiong X, Buekens P, Fraser W, Beck J & Offenbacher S 2006. Periodontal disease and adverse pregnancy outcomes: a systematic review. BJOG: An International Journal of Obstetrics & Gynaecology 113:135-43.
- Ylöstalo P, Järvelin M, Laitinen J & Knuuttila M 2006. Gingivitis, dental caries and tooth loss: risk factors for cardiovascular diseases or indicators of elevated health risks. Journal of Clinical Periodontology 33:92-101.

