Key messages
- About 1.1 million hospitalisations took place for Aboriginal and Torres Strait Islander people between July 2017 and June 2019, or an average of about 550,000 hospitalisations annually.
- Between July 2017 and June 2019, 44% of all hospitalisations for Indigenous Australians were for care involving dialysis. After dialysis, the next most common principal diagnoses were due to injury and poisoning (6.8% of hospitalisations), symptoms, signs and abnormal clinical and laboratory findings not elsewhere classified (5.7%), and respiratory diseases (5.4%),
- Between 2006–08 and 2017–19, the number of hospitalisations of Indigenous Australians approximately doubled, with an increase of 554,285 hospitalisations. Of this, nearly half (46%, or 252,612) was due to an increase in hospitalisations for care involving dialysis over the period.
- Excluding dialysis, the number of hospitalisations for Indigenous Australians increased by 301,673 between 2006–08 and 2017–19. The diagnosis groups contributing most to this increase were symptoms, signs and abnormal findings not elsewhere classified (accounting for 13% of the increase), injury and poisoning (11%), and respiratory diseases (9%).
- Hospitalisation rates for Indigenous Australians (excluding dialysis) were highest in Remote and Very remote areas between July 2017 and June 2019.
- Over the decade 2009–10 to 2018–19, the age-standardised rate of hospitalisation (excluding dialysis) increased by 46% for Indigenous Australians.
- Primary health care can play a pivotal role in helping to reduce health inequalities and hospitalisation rates. For example, research shows that optimal primary health care access in the Northern Territory has reduced hospitalisation significantly.
- Research has shown that primary care in remote Indigenous communities was associated with cost-savings to public hospitals and health benefits to individual patients.
- Research suggests that the high prevalence of chronic diseases experienced by Indigenous Australians and lack of chronic disease management support and out-of-hospital palliative care has resulted in high hospitalisation rates.
Why is it important?
Hospitalisation rates indicate the occurrence in a population of serious acute illnesses or conditions that require hospital treatment, and the access to and use of hospital treatment by people with such conditions. Hospitalisation rates for a particular disease do not directly indicate the level of occurrence of that disease in the population. Rates of hospitalisation are also impacted by access to primary care services (see measure 3.07 Selected potentially preventable hospital admissions) and other health services.
Hospitalisation rates are based on the number of hospital episodes of care rather than on the number of individual people who are hospitalised. A person who has frequent hospitalisations for the same disease is counted multiple times in the hospitalisation rate. For example, each kidney dialysis treatment is counted as a separate hospital episode, so that each person receiving three dialysis treatments per week contributes about 150 hospital episodes per year. Therefore, it is important to separate hospitalisation rates for dialysis from rates for other conditions. This is indicated in the ‘Findings’ section of this measure.
Each hospitalisation involves a principal diagnosis (that is, the problem that was chiefly responsible for the patient's episode of care) and additional diagnoses where applicable (that is, conditions or complaints either coexisting or arising during care). This report focuses on the principal diagnosis for each hospitalisation.
Hospitalisation data feature across multiple measures. This measure provides an overview of hospital admissions for Aboriginal and Torres Strait Islander people to serve as an introduction to other measures which provide more detail on the interaction between Indigenous Australians and the hospital sector. Tier 3 measures on health system performance (such as measure 3.06 Access to hospital procedures, measure 3.09 Self-discharge from hospital and measure 3.14 Access to services compared with need) provide further insight into Indigenous Australians’ access to the hospital sector, experience within the sector and barriers to accessing specific hospital services.
There are some instances where the gap in hospitalisation rates between Indigenous and non-Indigenous Australians is reported and this should be treated with caution. For hospitalisation data, this gap can be useful in understanding and comparing access to services. However, unlike many health outcomes, this gap does not necessarily reflect a disparity that needs to be closed in the short to medium term, particularly if it reflects where services are better addressing previously unmet need.
The National Aboriginal and Torres Strait Islander Health Plan 2021–2031 (the Health Plan), released in December 2021, provides a strong overarching policy framework for Aboriginal and Torres Strait Islander health and wellbeing and is the first national health document to address the health targets and priority reforms of the National Agreement on Closing the Gap. Priority 9 of the Health Plan focuses on improving access to person-centred and family-centred care. Early access to responsive primary care, and addressing barriers to accessing care, are identified by the Health Plan as key to addressing high hospitalisation rates of Indigenous Australians, where presentation often occurs at a later stage of disease.
The barriers to accessing care include racism, lack of cultural safety and lack of local cultural awareness among mainstream services, as well as cost, transport, communication pathways, service infrastructure and information capability. Person-centred care involves placing the experience of Indigenous Australian patients at the centre of determining responsive care so patients can determine their own health priorities and care pathways, this includes embedding trauma-aware and healing-informed approaches to care. Providing access to flexible, culturally safe and responsive acute care requires services to work with communities to understand their needs and to address the systemic factors that result in patients taking own leave or discharging against medical advice.
Data findings
Between July 2017 and June 2019, there were about 1.1 million hospitalisations for Indigenous Australians (including dialysis) (1,089,336 hospitalisations), corresponding to a rate of 656 per 1,000 population (Table D1.02.5). Excluding dialysis, there were 613,665 hospitalisations for Indigenous Australians, at a rate of 369 per 1,000 (Table D1.02.1, Table D1.02.5).
Top reasons for total hospitalisations
Between July 2017 and June 2019, the leading cause of hospitalisation was care involving dialysis (475,671 hospitalisations), which accounted for 44% of all hospitalisations for Indigenous Australians.
Dialysis is an artificial way to remove waste and excess water from the blood and regulate safe levels of circulating agents in the body, a function usually performed by the kidney. It is most often provided to treat chronic kidney failure but is sometimes needed in cases of acute kidney failure, where the kidneys have been temporarily damaged due to illness or injury. Most people undergoing dialysis attend three sessions per week (AIHW 2022a). Hospitalisation data count the number of dialysis episodes rather than the number of people who receive dialysis.
Among Indigenous Australians, after dialysis, the next four leading reasons for hospitalisation were:
- injury and poisoning (73,641, 6.8% of all hospitalisations for Indigenous Australians, or 12% of hospitalisations excluding dialysis): for example, fractures, wounds, burns or poisoning due to drugs. See also measure 1.03 Injury and poisoning.
- symptoms, signs and abnormal findings not elsewhere classified (62,306, 5.7% of all hospitalisations or 10% excluding dialysis): this includes symptoms such as abnormalities of heartbeat, abnormalities of breathing, chest pain, nausea and vomiting, headache, and convulsions that are not attributable to a specific diagnosis based on the information available at the time of the care.
- respiratory system diseases (59,301, 5.4% of all hospitalisations or 9.7% excluding dialysis): includes conditions such as asthma, chronic obstructive pulmonary disease (COPD), influenza and pneumonia. See also measure 1.04 Respiratory disease.
- pregnancy, childbirth and the puerperium (57,262, 5.3% or 9.3% excluding dialysis) (Table D1.02.5, Figure 1.02.1).
Figure 1.02.1: Hospitalisations for Indigenous Australians, by principal diagnosis, Australia, July 2017 to June 2019
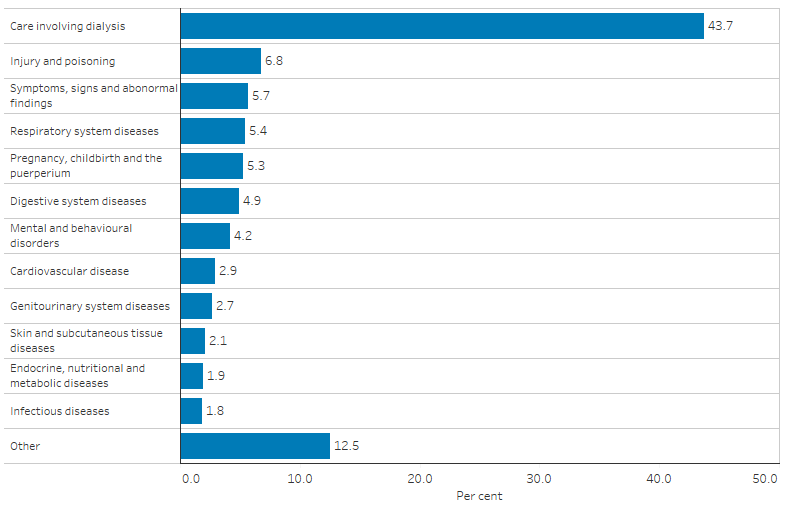
Note: See Table D1.02.5 for the ICD-10-AM codes included in each principal diagnosis grouping.
Source: Table D1.02.5. AIHW analysis of National Hospital Morbidity Database.
Where care involving dialysis was the principal diagnosis of hospitalisation for Indigenous Australians, the leading additional diagnoses were endocrine, nutritional and metabolic diseases (present for 7.8% of all hospitalisations for care involving dialysis) followed by diseases of the genitourinary system (6.9%) (Table D1.02.6).
Hospitalisation by sex and age
Between July 2017 and June 2019, 58% of total hospitalisations among Indigenous Australians were for females (354,766 hospitalisations, excluding dialysis). Indigenous females were hospitalised at 1.4 times the rate of Indigenous males (427 and 312 per 1,000, respectively).
The hospitalisation rate was higher for Indigenous females than Indigenous males in all jurisdictions. The largest relative difference was in the Northern Territory, where the rate for females was 1.5 times the rate for males (638 and 428 per 1,000, respectively) (Table D1.02.1).
The hospitalisation rate was higher for Indigenous females than Indigenous males between the age groups 15–24 to 45–54 years, and was otherwise similar or slightly higher for Indigenous males (Table D1.02.2).
Indigenous children aged 0–4 had a hospitalisation rate of 322 hospitalisations per 1,000 population in the two-year period from July 2017 to June 2019. The hospitalisation rate was lower among those aged 5–14 (109 per 1,000), then increased with age and was highest for those aged 65 and over (948 per 1,000) (Table D1.02.2, Figure 1.02.2).
Figure 1.02.2: Age-specific hospitalisation rates (excluding dialysis), by Indigenous status, Australia, July 2017 to June 2019
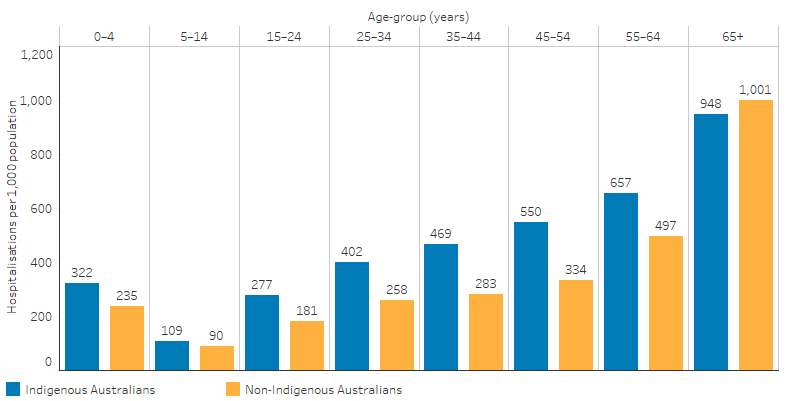
Source: Table D1.02.2. AIHW analysis of National Hospital Morbidity Database.
Looking at the top reasons for hospitalisation (excluding dialysis) by age group:
- Diseases of the respiratory system (26%) was the leading reason for hospitalisation for Indigenous Australians aged 0–4, followed by symptoms, signs and abnormal clinical and laboratory findings not elsewhere classified (9.1%), and certain infectious and parasitic diseases (9.0%).
- Among Indigenous children aged 5–14, injury and poisoning was the leading reason for hospitalisation (19%), followed by diseases of the respiratory and digestive systems (both 13%).
- For Indigenous Australians aged 15–24 and 25–44, pregnancy childbirth and the puerperium was the leading reason for hospitalisation (28% and 18%, respectively), followed by injury and poisoning (16% and 14%, respectively).
- Between the ages of 45–54 and 55–64, the leading reason for hospitalisation was symptoms, signs and abnormal clinical and laboratory findings not elsewhere classified (13% and 12%, respectively), followed by injury and poisoning for those aged 45–54 (11%) and respiratory diseases for those aged 55–64 (11%).
- Among Indigenous Australians aged 65 and over, the leading reason for hospitalisations were diseases of the respiratory and cardiovascular (circulatory) systems (both 12%), followed by symptoms, signs and abnormal clinical and laboratory findings not elsewhere classified (11%) (Table D1.02.8).
Hospitalisation by state and territory
From July 2017 to June 2019, across states and territories, the highest hospitalisation rate for Indigenous Australians was in the Northern Territory (531 per 1,000), followed by Queensland (413 per 1,000) and Western Australia (382 per 1,000). The hospitalisation rate in the Northern Territory was 2.3 times the rate in Tasmania (231 per 1,000), where the rate was the lowest (Table D1.02.1, Figure 1.02.3).
Figure 1.02.3: Hospitalisation rates (excluding dialysis) for Indigenous Australians, by state and territory, July 2017 to June 2019
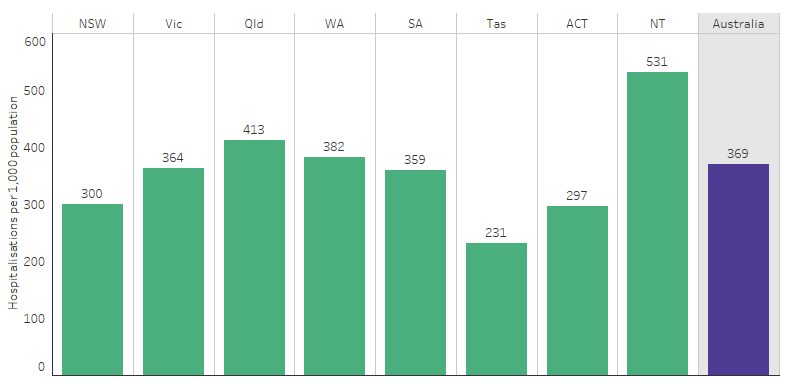
Source: Table D1.02.1. AIHW analysis of National Hospital Morbidity Database.
Hospitalisation by remoteness
From July 2017 to June 2019, the hospitalisation rate for Indigenous Australians in remote areas (Remote and Very remote areas combined) was 1.4 times the rate in non-remote areas (Major cities, Inner and Outer regional areas combined) (482 per 1,000 compared with 339 per 1,000) (Table 1.02.13, Figure 1.02.4).
Figure 1.02.4: Hospitalisation rates (excluding dialysis) among Indigenous Australians, by remoteness, Australia, July 2017 to June 2019
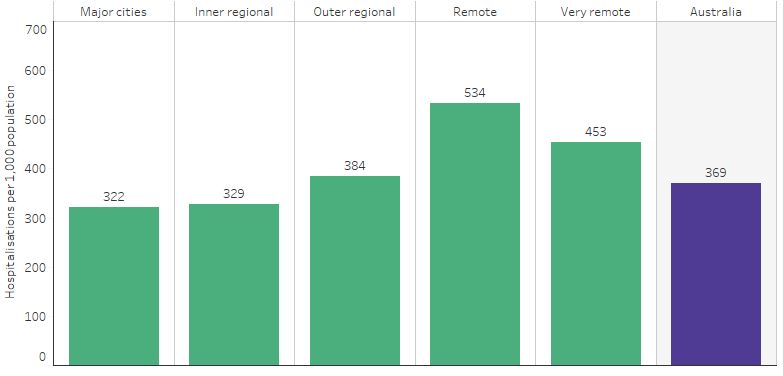
Source: Table D1.02.3. AIHW analysis of National Hospital Morbidity Database.
This pattern was the same in most states and territories (ranging from 1.2 to 1.5 times as high in remote areas as non-remote areas), excluding Tasmania, where the hospitalisation rate was higher for Indigenous Australians living in non-remote areas, and excluding Queensland, where the rate was similar in remote and non-remote areas (Table D1.02.13).
Same-day and overnight hospitalisation
Over the period July 2017 to June 2019, there were 703,999 same-day hospitalisations including dialysis for Indigenous Australians, corresponding to a rate of 424 per 1,000 population. Care involving dialysis was the most common reason for same-day hospitalisations, accounting for about two-thirds of these hospitalisations (67%, or 474,006) (based on principal diagnosis). The rate of same-day hospitalisations among Indigenous Australians excluding dialysis was 138 per 1,000.
Symptoms, signs and abnormal clinical and laboratory findings not elsewhere classified was the next leading reason for same-day hospitalisation for Indigenous Australians (a rate of 18 per 1,000; 4.3% of same-day hospitalisations), followed by injury, poisoning and other external causes (16 per 1,000; 3.9%) and digestive system diseases (14 per 1,000; 3.4%) (based on principal diagnosis) (Table D1.02.11).
Over the period July 2017 to June 2019, there were 385,337 overnight hospitalisations (including dialysis) for Indigenous Australians, a rate of 232 per 1,000. Dialysis accounted for a smaller proportion of overnight hospitalisations for Indigenous Australians (0.4%, 1,665 hospitalisations) than same-day hospitalisations (67%).
The top reason for overnight hospitalisations for Indigenous Australians was respiratory diseases (29 per 1,000 population; 13% of overnight hospitalisations), followed by injury and poisoning (28 per 1,000; 12%) and mental and behavioural disorders (20 per 1,000; 8.6%).
Pregnancy, childbirth and the puerperium was also a top reason for overnight hospitalisations for Indigenous women (47 per 1,000 female population; 10% of total hospitalisations for Indigenous Australians) (Table D1.02.12).
Comparisons with non-Indigenous Australians
Gaps in hospitalisation rates between Indigenous and non-Indigenous Australians should be treated with caution. For hospitalisation data, this gap can be useful in understanding and comparing access to services. However, unlike many health outcomes, this gap does not necessarily reflect a disparity that needs to be closed in the short to medium term, particularly if it reflects where services are better addressing previously unmet need.
From July 2017 to June 2019, after adjusting for differences in the age structure between the two populations, Indigenous Australians were hospitalised at 2.3 times the rate of non-Indigenous Australians when care involving dialysis was included, and 1.3 times the rate when dialysis was excluded (Table D1.02.5).
Hospitalisation rates (excluding dialysis) were higher for Indigenous Australians than non-Indigenous Australians in all age groups below 65 years. The greatest absolute difference was for those aged 45–54 (216 per 1,000) (Table D1.02.2, Figure 1.02.2).
From July 2017 to June 2019, excluding dialysis and after adjusting for differences in age structure:
- Indigenous males were hospitalised at 1.3 times the rate of non-Indigenous males and Indigenous females were hospitalised at 1.4 times the rate of non-Indigenous females (Table D1.02.2).
- All jurisdictions, except Tasmania, had a higher hospitalisation rate for Indigenous Australians than non-Indigenous Australians, with the highest in the Northern Territory (1.6 times the non-Indigenous rate) (Table D1.02.1).
- The hospitalisation rate for Indigenous Australians was 1.9 times the rate for non-Indigenous Australians in Remote areas, the highest rate ratio across remoteness areas. In Major cities and Inner regional areas, the rates for Indigenous Australians were 1.2 times the rate for non-Indigenous Australians in both cases, the lowest rate ratios across remoteness areas (Table D1.02.3).
The rate of same-day hospitalisations among Indigenous Australians (including dialysis) was 2.7 times the rate for non-Indigenous Australians (age-standardised). However, excluding dialysis, the rate for Indigenous Australians was lower: 0.9 times the rate for non-Indigenous Australians.
The leading principal diagnosis for same-day hospitalisations was dialysis for both Indigenous and non-Indigenous Australians (67% and 19%, respectively). This was followed by:
- symptoms, signs and abnormal clinical and laboratory findings not elsewhere classified (4.3% of same-day hospitalisations) and injury and poisoning (3.9%) for Indigenous Australians.
- Digestive system diseases (10%) and symptoms, signs and abnormal clinical and laboratory findings not elsewhere classified (8.8%) for non-Indigenous Australians.
For Indigenous Australians, the rate of same-day hospitalisations for dialysis was 11 times the rate for non-Indigenous Australians (the highest rate ratio of all causes), followed by injury and poisoning (1.7 times the rate for non-Indigenous Australians), respiratory diseases and pregnancy and childbirth (both 1.6 times the rate for non-Indigenous Australians) (Table D1.02.11).
Overnight hospitalisations (including dialysis) for Indigenous Australians were 1.9 times the rate for non-Indigenous Australians, after adjusting for age. The leading diagnoses for overnight hospitalisations:
- for Indigenous Australians was respiratory diseases (13% of overnight hospitalisations), followed by injury and poisoning (12%) and pregnancy and childbirth (10%).
- For non-Indigenous Australians was injury and poisoning (11%), followed by cardiovascular (circulatory) diseases (9.7%) and digestive system diseases (9.3%).
The rate of overnight hospitalisations for diseases of the skin for Indigenous Australians was 3.3 times the rate for non-Indigenous Australians (the highest rate ratio of all causes), followed by certain infectious diseases (3.1 times the rate for non-Indigenous Australians) and respiratory diseases (2.7 times the rate for non-Indigenous Australians) (Table D1.02.12).
Changes in hospitalisations over time
Information in this section includes the six jurisdictions where the quality of Indigenous identification in the hospitals data was considered of adequate quality over the combined time period: New South Wales, Victoria, Queensland, Western Australia, South Australia and the Northern Territory.
Between 2006–08 and 2017–19, the number of hospitalisations for Indigenous Australians approximately doubled, with an increase of 554,285 hospitalisations between the two periods. Care involving dialysis accounted for 46% (252,612 hospitalisations) of this increase.
Excluding dialysis, the number of hospitalisations for Indigenous Australians increased by 301,673 between 2006–08 and 2017–19. Of this increase:
- 13% (38,854) was for symptoms, signs and abnormal clinical and laboratory findings not elsewhere classified,
- 11% (33,148) was for injury and poisoning,
- 9.0% (27,097) was for diseases of the respiratory system, and
- 5.9% (17,820) was for pregnancy, childbirth and the puerperium (Table D1.02.9).
Over the decade 2009–10 to 2018–19, after adjusting for differences in the age structure between the two populations, the hospitalisation rate (excluding dialysis) increased by 46% for Indigenous Australians and by 13% for non-Indigenous Australians. Over the same period, this resulted in a widening of the rate difference (absolute gap) (from 16.1 in 2009–10 to 131.7 in 2018–19) and the ratio of the hospitalisation rate for Indigenous Australians to the rate for non-Indigenous Australians (from a rate ratio of 1.1 in 2009–10 to 1.4 in 2018–19) (Table D1.02.4, Figure 1.02.5).
Figure 1.02.5: Trends in age-standardised hospitalisation rates (excluding dialysis), by Indigenous status, NSW, Vic, Qld, WA, SA and NT, 2006–07 to 2018–2019
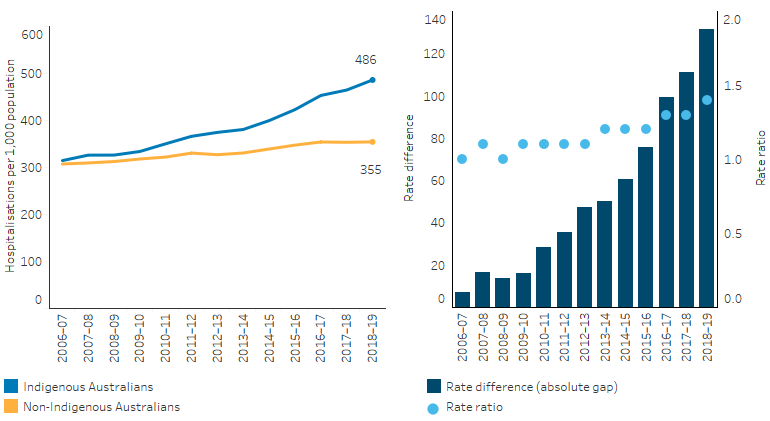
Note: Rate difference is the age-standardised rate (per 1,000) for Indigenous Australians minus the age-standardised rate (per 1,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: D1.02.4. AIHW analysis of National Hospital Morbidity Database.
Research and evaluation findings
In Australia, hospital services are provided by both public and private hospitals. Hospitals provide a range of services for admitted patients (elective care, maternity services and medical and surgical services). Non-admitted patient services are mostly located in public hospitals and include emergency department services and outpatient clinics (AIHW 2022b). Primary health care can play a pivotal role in closing the gap in Indigenous health and helping to lower health inequalities and hospitalisation rates. Aboriginal Community Controlled Health Services and other Indigenous specific primary health care deliver culturally appropriate primary health care across Australia, however many Indigenous Australians must, or choose to, access health care through mainstream services (DoH 2017).
Research shows that optimal primary health care access in the Northern Territory has reduced hospitalisation significantly (Zhao Y. et al. 2013). Primary care in remote Indigenous communities was also shown to be associated with cost-savings to public hospitals and health benefits to individual patients (Zhao Y et al. 2014). Evidence suggests that access to primary health care can be improved when it is tailored to the needs of, and owned or managed by, Indigenous Australians (Davy et al. 2016).
In 2017, the Australian Government released My Life My Lead - Opportunities for strengthening approaches to the social determinants and cultural determinants of Indigenous health: Report on the national consultations (My Life, My Lead). These consultations provided an opportunity for Indigenous communities and leaders, governments, non‑government and the private sector to inform the refresh of the National Aboriginal and Torres Strait Islander Health Plan 2013–2023, which led to the National Aboriginal and Torres Strait Islander Health Plan 2021–2031. The My Life My Lead consultations highlighted that although there have been significant health gains, poor access to health services contributes to the significant health inequities still experienced by Indigenous Australians (DoH 2017). Although hospitalisation rates are higher for Indigenous Australians than non-Indigenous Australians, they do not access health services to the level expected given their relatively poorer health status. This is partly due to an inadequate supply of Indigenous primary health care services and an inequitable share of mainstream programs. While Indigenous Australians under-utilise mainstream health services and many prefer Indigenous-specific services, mainstream government expenditure still dominates health expenditure for Indigenous Australians (Alford 2014).
Across Australia there is a growing need for out-of-hospital palliative and chronic disease care, a lack of which is leading to an overuse of hospitals. In addition, the high prevalence of chronic diseases and limited access to primary services experienced by many Indigenous Australians has resulted in high hospitalisation rates. There are limited respite services for palliative care patients in the Northern Territory. The establishment of a flexible, community-based and culturally appropriate palliative and chronic disease respite facility in Alice Springs resulted in a reduction in local hospital admissions (Carey et al. 2017).
Several studies have linked multi-morbidity to an increased use of health services, particularly in hospitalisation (Gruneir. et al. 2016). It is therefore consistent that hospitalisation rates are higher amongst Indigenous Australians compared with non-Indigenous Australians, given that prevalence of multi-morbidity is higher amongst Indigenous Australians than non-Indigenous Australians (Hussain et al. 2018):
- A recent study, based on the New South Wales hospital data, found that, after adjusting for age, sex, and socioeconomic status, the prevalence of multi-morbidity among Indigenous Australians was 2.6 times that of non-Indigenous Australians. This difference accounted for a large proportion of the difference in mortality rates between the two groups of patients.
- The prevalence of multi-morbidity was higher among Indigenous Australians in all age groups. In younger age groups this was because of the higher prevalence of mental health conditions, while in the older age group (over 60 years) it was because of physical health conditions (Broe & Radford 2018).
Research by Harrold and others (2014) found that the rate of preventable hospitalisations was 2.16 times higher for Indigenous Australians compared with non-Indigenous Australians who lived in the same Statistical Local Area in New South Wales, after controlling for age and sex. The disparity is greatest in rural and remote areas relative to major cities. The largest differences in preventable hospitalisations were for diabetes, chronic obstructive pulmonary disease and rheumatic heart disease. The authors suggested that differences in preventable hospitalisation rates between the Indigenous and non-Indigenous population may be due to less availability of assistance and care at home, greater disease disparity, and access to primary health care. Despite the disparity, the researchers suggested that there is potential to reduce preventable hospitalisations (Harrold et al. 2014).
Lower access to hospitals and health services can lead to poorer health outcomes. Findings of a project that examined spatial variation in Indigenous Australian women’s access to hospitals with public birthing services and three other types of maternal health services across Australia found that the lowest levels of access to maternal health services are in Remote and Very remote areas. Poorer access to maternal health services is associated with higher rates of pre-term birth and low birthweight (AIHW 2017).
Implications
Given the high burden of disease, high prevalence of many health conditions and high death rates for Indigenous Australians, it is clear that the health system is not meeting the level of need for health care for Indigenous Australians. This points to a broader issue of access to care, explored further in measure 3.14 Access to services compared with need.
Given the high proportion of hospitalisations for Indigenous Australians requiring dialysis (44%), more attention should be given to alternatives that can provide dialysis outside of the hospital system. Innovative use of mobile dialysis units in South Australia and Central Australia have reduced disruption to patients by allowing them to receive treatment closer to home (albeit for short periods), and also have the potential to reduce hospitalisations (Conway et al. 2018; Western Desert Nganampa Walytja Palyantjaku Tjutaku Aboriginal Corporation).
The high rates of infectious diseases, including skin conditions, suggests that addressing the social determinants of health such as overcrowded housing and other environmental factors in Indigenous communities will help to reduce the disease burden, and the associated hospitalisations.
Strategies to improve hospital service delivery to Indigenous Australians by improving access and removing barriers to hospital services will improve the patient journey through the health system and improve outcomes for Indigenous Australians. As stated in the Health Plan, providing access to flexible, culturally safe and responsive acute care requires services to work with communities to understand their needs and to address the systemic factors (such as racism and lack of cultural safety) that result in patients taking own leave or discharging against medical advice. Furthermore, providing access to culturally safe primary health care can also reduce the costs associated with hospitalisations, and yield health benefits to patients.
The Health Plan is the overarching policy framework to drive progress against the Closing the Gap health targets and priority reforms. Implementation of the Health Plan aims to drive structural reform towards models of care that are prevention and early intervention focused, with greater integration of care systems and pathways across primary, secondary and tertiary care. It also emphasises the need for mainstream services to address racism and provide culturally safe and responsive care and be accountable to Aboriginal and Torres Strait Islander people and communities.
Although hospitalisation rates are higher for Indigenous Australians than non-Indigenous Australians, they do not access health services to the level expected given their relatively poorer health status. As stated earlier, this is partly due to an inadequate supply of Indigenous primary health care services and an inequitable share of mainstream programs. Aboriginal Community Controlled Health Services and other Indigenous specific primary health care deliver culturally appropriate primary health care across Australia and this plays a vital role in preventing otherwise preventable hospital admissions.
As part of the National Agreement on Closing the Gap, the health sector was identified as one of four initial sectors for joint national strengthening effort and the development of a three-year Sector Strengthening Plan. The Health Sector Strengthening Plan (Health-SSP) was developed in 2021, to acknowledge and respond to the scope of key challenges for the sector, providing 17 transformative sector strengthening actions. Developed in partnership with the Aboriginal and Torres Strait Islander community-controlled health sector and other Aboriginal and Torres Strait Islander health organisations, the Health-SSP will be used to prioritise, partner and negotiate beneficial sector-strengthening strategies.
The policy context is at Policies and strategies.
References
-
AIHW (Australian Insitute of Health and Welfare) 2013. Indigenous identification in hospital separations data: quality report. Canberra: AIHW.
-
AIHW 2017. Spatial Variation in Aboriginal and Torres Strait Islander Women's Access to 4 Types of Maternal Health Services. Canberra AIHW.
-
AIHW 2022a. Chronic kidney disease: Australian facts. Canberra: Australian Institute of Health and Welfare. Viewed 29/09/2022.
-
AIHW 2022b. Australia's hospitals at a glance. Canberra: AIHW. Viewed 28 July 2022.
-
Alford K 2014. Investing in Aboriginal community controlled health makes economic sense. Canberra: National Aboriginal Community Controlled Health Organisation.
-
Broe G & Radford K 2018. Multimorbidity in Aboriginal and non-Aboriginal people. Medical Journal of Australia 209:16-7.
-
Carey TA, Arundell M, Schouten K, Humphreys JS, Miegel F, Murphy S et al. 2017. Reducing hospital admissions in remote Australia through the establishment of a palliative and chronic disease respite facility. BMC Palliative Care 16:54.
-
Conway J, Lawn S, Crail S & McDonald S 2018. Indigenous patient experiences of returning to country: a qualitative evaluation on the Country Health SA Dialysis bus. BMC health services research 18:1010.
-
Davidson L, Knight J & Bowen A 2020. Skin infections in Australian Aboriginal children: a narrative review. Medical Journal of Australia 212:231-7.
-
Davy C, Harfield S, McArthur A, Munn Z & Brown A 2016. Access to primary health care services for Indigenous peoples: A framework synthesis. International Journal for Equity in Health 15:163.
-
DoH (Department of Health) 2017. My Life My Lead - Opportunities for strengthening approaches to the social determinants and cultural determinants of Indigenous health: Report on the national consultations. Canberra
-
Gruneir. A, Bronskill. SE, Maxwell. CJ, Bai. YQ, Kone. AJ, Thavorn. K et al. 2016. The association between multimorbidity and hospitalisation is modified by individual demographics and physician continuity of care: a retrospective cohort. BMC health services research 16.
-
Harrold T, Randall D, Falster M, Lujic S & Jorm L 2014. The Contribution of Geography to Disparities in Preventable Hospitalisations between Indigenous and Non-Indigenous Australians. PloS one.
-
Hendrickx D, Stephen A, Lehmann D, Silva D, Boelaert M, Carapetis J et al. 2016. A systematic review of the evidence that swimming pools improve health and wellbeing in remote Aboriginal communities in Australia. Australian & New Zealand Journal of Public Health 40:30-6.
-
Hussain M, Katzenellenbogen J, Sanfilippo F, Murray K & Thompson S 2018. Complexity in disease management: A linked data analysis of multimorbidity in Aboriginal and non-Aboriginal patients hospitalised with atherothrombotic disease in Western Australia. PloS one 3(8): e0201496.
-
Western Desert Nganampa Walytja Palyantjaku Tjutaku Aboriginal Corporation. The Purple Truck.
-
Zhao Y, Thomas S, Guthridge S & Wakerman J 2014. Better health outcomes at lower costs: the benefits of primary care utilisation for chronic disease management in remote Indigenous communities in Australia's Northern Territory. BMC health services research 14:463.
-
Zhao Y, Wright J, Guthridge SL & Lawton P 2013. The relationship between number of primary health care visits and hospitalisations: evidence from linked clinic and hospital data for remote Indigenous Australians. BMC health services research 13:466.

