Key messages
- Between July 2019 and June 2021, the proportion of hospitalisations for Aboriginal and Torres Strait Islander (First Nations) people that had a procedure recorded was 12 percentage points lower than for non-Indigenous Australians, based on age-standardised percentages (66% compared with 78%).
- Over the decade from 2011–12 to 2020–21, based on age-standardised rates, there was a 19% increase in hospitalisations of First Nations people where a procedure was recorded. The gap in procedure rates between First Nations people and non-Indigenous Australians narrowed over this period.
- For First Nations people, the proportion of hospitalisations between July 2019 and June 2021 with a procedure recorded was highest for those living in Tasmania (78%), followed by New South Wales and Victoria (both 71%), Western Australia and South Australia (both 66%) and the lowest for the Northern Territory (56%).
- For First Nations people, the proportion of hospitalisations with a procedure recorded decreased with increasing remoteness, from 70% for those living in Major cities and Inner regional areas to 56% for those living in Very remote areas.
- Research has revealed that First Nations people face multiple barriers at every point in the surgical journey, including the lack of culturally safe care, lower access to specialist services and elective surgery, and poorer surgical outcomes (due to factors such as presenting at more advanced stages of disease).
- Timely diagnosis and treatment are critical for preventing death from coronary heart disease. In the 2-year period from July 2019 to June 2021, 49% of hospitalisations for coronary heart disease among First Nations people included coronary angiography, and 30% of those included a revascularisation procedure. The age-standardised rates of both coronary angiography and revascularisations procedures for First Nations people were 0.8 times lower compared to non-Indigenous Australians.
- First Nations people have a much greater risk of developing end-stage kidney disease compared with non-Indigenous Australians, but are less likely to receive a kidney transplant. Contributing factors to lower procedure rates include healthcare system inefficiencies in the assessment, screening and clearance process (such as for cardiac, malignancy, respiratory and dental issues), and delays in investigations or clinical reviews.
- Improving the cultural safety of hospital environments is integral to improving health outcomes for First Nations people, as they are more likely to seek access to health care and have better outcomes if there are culturally safe and respectful services. Monitoring of Cultural Safety in Health Care for First Nations people is limited by a lack of national and state-level data.
- The Lighthouse Hospital Project has found that some key initiatives have led to improvements in care such as the expansion of the Aboriginal Health Workforce, better Indigenous status identification of patients, engaging in effective partnerships with First Nations communities, fostering champions among clinical staff, patient-centred care and improved communication.
Why is it important?
Australians with illnesses that can be effectively treated by hospital-based medical and surgical procedures should have equitable access to these procedures. Aboriginal and Torres Strait Islander (First Nations) people are more likely to be hospitalised than other Australians, but less likely to receive a medical or surgical procedure while in hospital (ABS & AIHW 2008; Cunningham 2002; O'Brien P et al. 2021; Westphal et al. 2019). The disparities relating to this are not always explained by diagnosis, age, sex or place of residence and are apparent in public but not private hospitals (Cunningham 2002).
Patients suspected of having heart disease should receive appropriate and timely diagnostic services (AIHW 2021a). For patients admitted to hospital with coronary heart disease, access to coronary angiography (a procedure used to detect coronary artery blockage) can be important in the diagnosis and establishment of a treatment plan. Coronary heart disease may be treated with pharmacotherapy or through repairing the heart’s blood vessels, either using a medical procedure (percutaneous coronary interventions) or a surgical procedure (coronary artery bypass grafts).
Studies have found that First Nations patients were less likely to receive a coronary angiography than non-Indigenous Australians, after controlling for age, comorbidities and remoteness (Tavella et al. 2016) (see measure 1.05 Cardiovascular disease).
First Nations people have a much greater risk of developing end-stage kidney disease compared with non-Indigenous Australians, but are less likely to receive a kidney transplant (The Transplantation Society of Australia and New Zealand 2019). First Nations patients were also less likely to be added to the kidney transplantation waiting list during the first year of renal replacement therapy, irrespective of differences in patient- or disease-related factors (Khanal et al. 2018). First Nations patients who receive a kidney transplant wait longer for an organ donor than non-Indigenous patients and experience significantly worse post-transplant outcomes (see measure 1.10 Kidney disease).
Several studies have shown that First Nations people have a poorer survival rate for cancer. This is partly explained by later diagnosis and referral for specialist treatment (Condon et al. 2006; Valery et al. 2006). However, after controlling for the stage of diagnosis, First Nations people are less likely to have treatment for cancer (for example, surgery, chemotherapy or radiotherapy), tend to wait longer for surgery and have lower survival rates for many cancers (Hall et al. 2004; Valery et al. 2006) (see measure 1.08 Cancer).
There is considerable evidence that poor outcomes in hospitals and health care facilities for First Nations people are related to systemic or institutionalised racism (Bourke et al. 2019; Henry et al. 2004; Malatzky et al. 2020). Improving the cultural safety of hospital environments is integral to improving health outcomes for First Nations people, as they are more likely to seek access to health care and have better outcomes if there are culturally safe and respectful services available (Congress of Aboriginal and Torres Strait Islander Nurses and Midwives 2016). Institutional resistance may require organisational change mandated by standards (Laverty et al. 2017).
The National Aboriginal and Torres Strait Islander Health Plan 2021–2031 (the Health Plan), provides a strong overarching policy framework for First Nations health and wellbeing and is the first national health document to address the health targets and priority reforms of the National Agreement on Closing the Gap. Improving the health system is a key focus of the Health Plan which includes:
- Priority 8: Identify and eliminate racism, including individual and institutional racism across health, disability and aged care systems
- Priority 9: Access to person-centred and family-centred care, including making acute care settings accessible and culturally safe to address gaps such as those seen in surgery procedures and wait times, and in rates of discharge against medical advice.
The Health Plan is discussed further in the Implications section of this measure.
Data findings
A procedure in this measure refers to a clinical intervention that is surgical in nature, carries a procedural and anaesthetic risk, requires specialised training, and/or requires special facilities or equipment only available in an acute care setting. Procedures therefore encompass surgical procedures as well as non-surgical investigative and therapeutic procedures (AIHW 2022b).
From July 2019 to June 2021, 66% (444,091) of hospitalisations (excluding dialysis) for First Nations people had a procedure recorded. The proportion of hospitalisations with a procedure recorded was similar between First Nations males (66%) and First Nations females (65%) (Table D3.06.1).
After adjusting for differences in the age structure between the First Nations and non-Indigenous populations, the proportion of hospitalisations for First Nations people that included a procedure was also lower than that for non-Indigenous Australians (age-standardised percentage of 66% compared with 78%, rate ratio 0.8) (Table D3.06.1). Age-specific rates of procedures while in hospital show somewhat higher rates in older age groups (Figure 3.06.1). Throughout this measure, age-standardised rates are generally used for comparisons by Indigenous status (for all ages combined); however, crude rates for both First Nations people and non-Indigenous Australians are available in the data tables.
Hospital sector
In the period 2019–21, 87% of total hospitalisations (including dialysis) for First Nations people occurred in public hospitals (AIHW 2021c, 2022b). Between July 2019 and June 2021, 63% (380,033) of hospitalisations for First Nations people in public hospitals had a procedure recorded, compared with 96% (64,058) of hospitalisations for First Nations people in private hospitals (Table D3.06.5). In the same period, 86% of the 444,091 hospitalisations for First Nations people with a procedure recorded took place in a public hospital (including psychiatric), and the remaining 14% in private hospitals (including in private free-standing day hospital facilities) (Table D3.06.6).
Hospital procedures by age group
Between July 2019 and June 2021, the proportion of hospitalisations for First Nations people where at least one procedure was performed was generally higher among older age groups:
- 56% for infants (aged under 1)
- between 60% and 65% for the age groups 1–14, 15–34 and 35–54
- 74% for those aged 55–64
- 79% for those aged 65 and over (Figure 3.06.1).
Across all age groups, First Nations people had lower proportions of hospitalisations that included a procedure compared with non-Indigenous Australians (Table D3.06.1, Figure 3.06.1).
Figure 3.06.1: Proportion of hospitalisations (excluding dialysis) with a procedure recorded, by Indigenous status and age group, Australia, July 2019 to June 2021
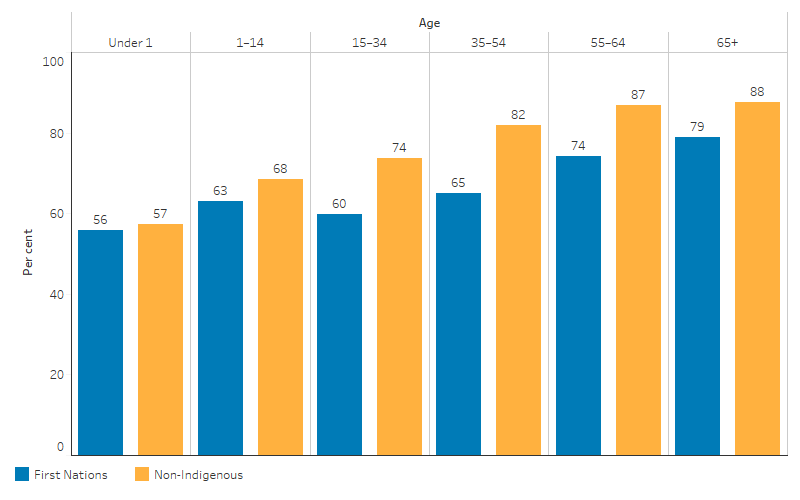
Source: Table D3.06.1. AIHW analysis of National Hospital Morbidity Database and ABS population estimates and projections (ABS 2019a, 2019b, 2022a, 2022b) for calculation of rates.
Hospital procedures by remoteness
Between July 2019 and June 2021, analysis across 5 remoteness areas shows that the proportion of hospitalisations with a procedure recorded was lower for First Nations people living in more remote areas. For First Nations people, the proportion of hospitalisations with a procedure recorded was highest for those living in Major cities (70%) and Inner regional areas (70%), followed by those living in Outer regional areas (64%), Remote areas (57%) and Very remote areas (56%). A similar pattern in the proportion of hospitalisations with a procedure recorded was observed for non-Indigenous Australians, with lower rates among residents of more remote areas (Table D3.06.1, Figure D3.06.2).
Figure 3.06.2: Proportion of hospitalisations (excluding dialysis) of First Nations people with a procedure recorded, by remoteness, Australia, July 2019 to June 2021
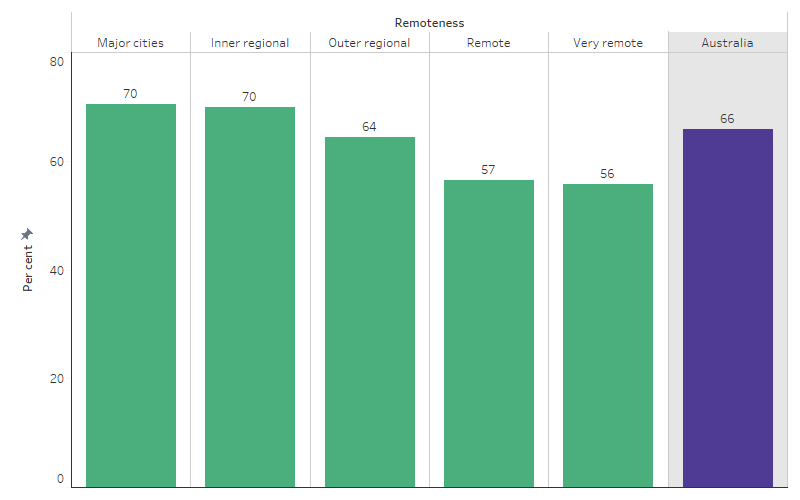
Source: Table D3.06.1. AIHW analysis of National Hospital Morbidity Database and ABS population estimates and projections (ABS 2019a, 2019b, 2022a, 2022b) for calculation of rates.
After adjusting for differences in the age structure between First Nations and non-Indigenous populations, the gap in the proportions of hospitalisations with a procedure recorded was largest for those living in Remote areas (age-standardised rate difference of 14.9 percentage points), followed by Very remote areas (11.7 percentage points) and smallest for those living in Major cities (7.7 percentage points) (Table D3.06.1).
Hospital procedures by state and territory
Between July 2019 and June 2021, the proportion of hospitalisations for First Nations people with a procedure recorded varied by state and territory. For First Nations people, the proportion of hospitalisations with a procedure recorded was highest for those living in Tasmania (78%), followed by New South Wales and Victoria (both 71%), Western Australia and South Australia (both 66%) and lowest for the Northern Territory (56%) (Table D3.06.1, Figure 3.06.3).
Figure 3.06.3: Proportion of hospitalisations (excluding dialysis) of First Nations people with a procedure recorded, by Jurisdiction, Australia, July 2019 to June 2021
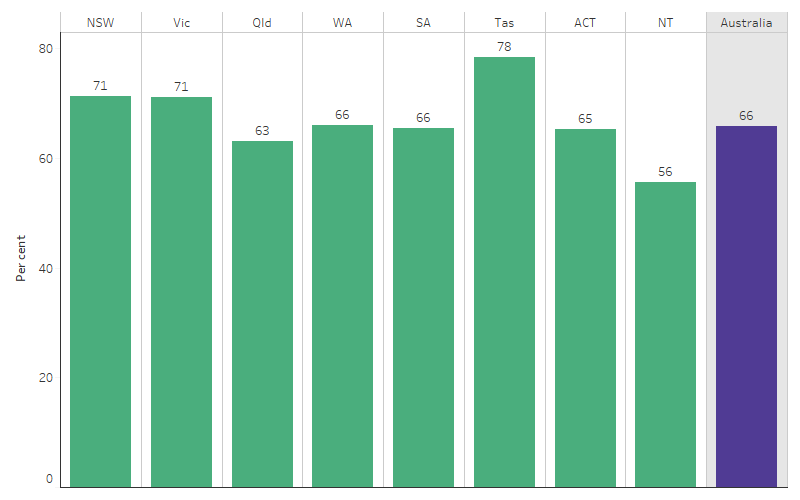
Source: Table D3.06.1. AIHW analysis of National Hospital Morbidity Database and ABS population estimates and projections (ABS 2019a, 2019b, 2022a, 2022b) for calculation of rates.
After adjusting for the differences in the age structure between the two populations, the proportion of hospitalisations that included a procedure was lower for First Nations people across all states and territories compared with non-Indigenous Australians, with the rate differences across the jurisdictions ranging from 1.8 percentage points (in Tasmania) to 17.5 percentage points (in Western Australia) (Table D3.06.1).
Principal diagnosis of hospital procedures
Table 3.06-1 shows the proportion of hospitalisations for First Nations people and non-Indigenous Australians that included a procedure by principal diagnosis (data shown are crude percentages). Principal diagnosis is based on chapters in the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM).
Between July 2019 and June 2021, the proportion of hospitalisations for First Nations people that included at least one procedure was highest for hospitalisations with a principal diagnosis of cancer and other neoplasms (94%), followed by diseases of the eye and adnexa (93%). Hospitalisations for First Nations people due to respiratory diseases, infectious and parasitic disorders were the least likely to include a procedure (52% and 44%, respectively) (excluding diagnoses of ‘symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified’). A similar pattern was observed for non-Indigenous Australians. However, the proportion of hospitalisations that included a procedure was higher for non-Indigenous Australians than First Nations people for every principal diagnosis category (ICD-10-AM chapters) except ‘Certain conditions originating in the perinatal period’ (Table 3.06-1, based on crude rates).
Between July 2019 and June 2021, hospitalisations with mental and behavioural disorders as a principal diagnosis had the largest absolute gap in procedure rates (rate difference of 16.9 percentage points) between First Nations people and non-Indigenous Australians (57% compared with 74%) (ranking excluding diagnoses of ‘symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified’). The next largest difference was for nervous system diseases (rate difference of 16.5 percentage points) – 68% for hospitalisations of First Nations people compared with 85% for non-Indigenous Australians (Table 3.06-1).
The smallest difference in procedure rates was for diseases of the ear and mastoid process (rate difference of 0.4 percentage points) – 81.6% of hospitalisations for diseases of the ear and mastoid process among First Nations people included a procedure, compared with 82.0% for non-Indigenous Australians (Table 3.06-1).
Table 3.06-1: Proportion of hospitalisations with a procedure reported, by principal diagnosis and Indigenous status, Australia, July 2019 to June 2021
| Principal diagnosis chapter (excluding dialysis) | First Nations (%) | Non-Indigenous (%) | Rate difference |
|---|---|---|---|
|
Cancer and other neoplasms (C00–D48) |
93.5 |
96.9 |
-3.4 |
|
Eye and adnexa diseases (H00–H59) |
93.2 |
98.5 |
-5.3 |
|
Diseases of the blood and blood-forming organs and certain disorders involving the immune mechanism (D50–D89) |
92.1 |
96.3 |
-4.2 |
|
Congenital malformations, deformations and chromosomal abnormalities (Q00–Q99) |
90.5 |
94.0 |
-3.5 |
|
Factors influencing health status and contact with health services (Z00–Z48, Z50–Z99) |
83.1 |
95.2 |
-12.1 |
|
Ear and mastoid process diseases (H60–H95) |
81.6 |
82.0 |
-0.4 |
|
Musculoskeletal system and connective tissue diseases (M00–M99) |
80.2 |
92.6 |
-12.4 |
|
Certain conditions originating in the perinatal period (P00–P96) |
79.4 |
76.6 |
2.8 |
|
Endocrine and nutritional and metabolic diseases (E00–E89) |
79.0 |
88.1 |
-9.0 |
|
Digestive diseases (K00–K93) |
74.1 |
88.7 |
-14.5 |
|
Cardiovascular diseases (I00–I99) |
71.3 |
81.0 |
-9.6 |
|
Nervous system diseases (G00–G99) |
68.4 |
84.9 |
-16.5 |
|
Skin and subcutaneous tissue diseases (L00–L99) |
66.9 |
73.9 |
-7.0 |
|
Genitourinary diseases (N00–N99) |
65.3 |
79.2 |
-14.0 |
|
Pregnancy, childbirth and the puerperium (O00–O99) |
64.9 |
75.4 |
-10.4 |
|
Injury, poisoning and certain other consequences of external causes (S00–T98) |
63.7 |
73.7 |
-10.0 |
|
Mental and behavioural disorders (F00–F99) |
57.3 |
74.2 |
-16.9 |
|
Respiratory diseases (J00–J99) |
51.7 |
67.7 |
-15.9 |
|
Certain infectious and parasitic diseases (A00–B99) |
44.3 |
53.9 |
-9.6 |
|
Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00–R99) |
39.8 |
61.1 |
-21.3 |
|
Any principal diagnosis |
65.8 |
82.7 |
-16.9 |
Note: Data are crude percentages.
Source: Table D3.06.2. AIHW analysis of National Hospital Morbidity Database.
Hospital procedures related to coronary heart disease
Timely diagnosis and treatment are critical for preventing death from coronary heart disease. Coronary angiography (x-ray imaging to detect narrowed or blocked blood vessels) and definitive revascularisation (refers to percutaneous coronary intervention or coronary artery bypass graft) procedures (surgery to overcome blockages) are essential forms of diagnosis and treatment for coronary heart diseases (AIHW 2021a).
Between July 2019 and June 2021, 49% of hospitalisations among First Nations people for coronary heart disease had a coronary angiography procedure performed, and 30% had a revascularisation procedure (based on crude rates) (Table D3.06.9).
After adjusting for differences in the age-structure between the two populations, the proportion of hospitalisations for coronary heart disease that included coronary angiography was lower for First Nations people than non-Indigenous Australians (age-standardised proportion of 47% compared with 56%; rate ratio 0.8), as was the rate of revascularisation procedures (29% compared with 33%; rate ratio 0.9) (Table D3.06.9, Figure 3.06.4).
Figure 3.06.4: Age-standardised proportion of hospitalisations for coronary heart disease where the patient received a coronary angiography or revascularisation procedure, by type of procedure and Indigenous status, Australia, July 2019 to June 2021
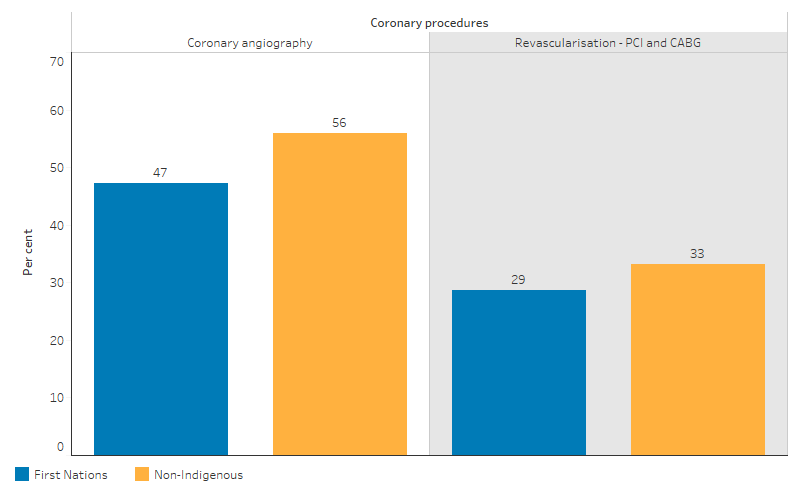
Source: Table D3.06.9. AIHW analysis of National Hospital Morbidity Database and ABS population estimates and projections (ABS 2019a, 2019b, 2022a, 2022b) for calculation of rates.
Acute coronary syndrome is a term that describes a range of conditions related to sudden, reduced blood flow to the heart including acute myocardial infarction (heart attack) and unstable angina (pressure in the chest while at rest or doing light physical activity) when first presented as clinical emergencies with chest pain or other features. In the following analysis of acute coronary syndrome, data are presented for ‘hospitalised events’, with adjustments made to reduce double-counting of hospitalisations for the same person associated with the same event of acute coronary syndrome (see AIHW 2021a for more detailed specifications). The results are based on the 3-year period between July 2017 and June 2020 combined and sourced from the Better Cardiac Care measures for Aboriginal and Torres Strait Islander people report (AIHW 2023b).
Among First Nations adults (aged 18 and over) between July 2017 and June 2020, the proportion of hospitalised events for acute coronary syndrome that included coronary angiography and/or a definitive revascularisation procedure was highest among those aged 18–34 (71%), which decreased for older age groups (to 48% for those aged 65 and over). The proportion of First Nations adults receiving these procedures for hospitalised acute coronary syndrome events was lower compared with non-Indigenous adults across all age groups, except for those aged 18–34 (71% for First Nations adults compared with 67% for non-Indigenous adults).
After adjusting for differences in the age structure between the two populations, the proportion of hospitalised acute coronary syndrome events that included coronary angiography or definitive revascularisation was 8.1 percentage points lower for First Nations people than for non-Indigenous Australians (63.4% compared with 71.5%, rate ratio of 0.9) (AIHW 2023b).
Across remoteness areas, for First Nations adults, the proportion of hospitalised events for acute coronary syndrome between July 2017 and June 2020 that included a coronary angiography and/or a definitive revascularisation procedure varied between 56% and 62% (62% for First Nations adults living in Outer regional areas; 61% in Very remote areas; 59% in both Major Cities and Remote areas; and 56% in Inner regional areas).
After adjusting for the differences in the age structure between the two populations, the proportions of hospitalised events for acute coronary syndrome that included coronary angiography and/or a definitive revascularisation procedure (age-standardised rates) were lower for First Nations people compared with non-Indigenous Australians in 4 of 5 remoteness areas (ranging from a rate difference of 2.8 percentage points in Outer regional areas to 10.0 percentage points in Major Cities). The exception was for First Nations people living in Remote areas of Australia where the proportion was slightly higher than that of non-Indigenous Australians (difference of 1.4 percentage points) (AIHW 2023b).
Factors influencing receiving a hospital procedure
A logistic regression analysis was performed to examine the factors associated with the likelihood of a First Nations people in hospital receiving a procedure between July 2019 and June 2021. After controlling for factors such as age group and principal diagnosis category, statistically significant factors associated with the likelihood of First Nations people receiving a procedure while in hospital included:
- whether the hospital was public or private (higher likelihood for private hospitals compared to public hospitals)
- the number of diagnoses recorded for a patient (higher likelihood for those with higher number of diagnoses)
- state and territory of usual residence (compared to New South Wales, a higher likelihood for those in Victoria and Tasmania, but lower for those in other states and territories)
- remoteness of usual residence (lower likelihood for those living in more remote areas compared to Major cities)
- sex (higher likelihood for males compared to females) (Table D3.06.13).
Changes over time
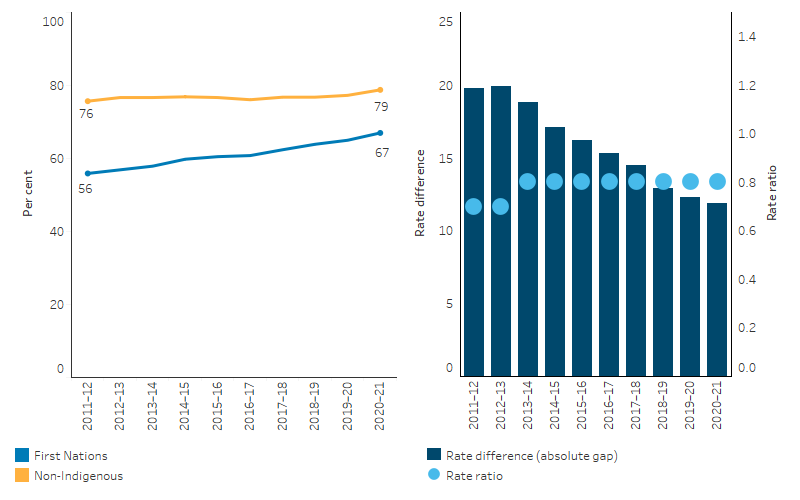
Over the decade from 2011–12 to 2020–21, based on linear regression, the age-standardised proportion of hospitalisations where a procedure was recorded increased by 19.0% for First Nations people and by 2.3% for non-Indigenous Australians. As a result, the absolute gap (rate difference) between First Nations people and non-Indigenous Australians in the proportion of hospitalisations where a procedure was recorded narrowed from a difference of 20 percentage points (in 2011–12) to a difference of 12 percentage points (in 2020–21) while relative gap (rate ratio) changed from 0.7 in 2011–12 to 0.8 in 2013–14 and remained same thereafter (Table D3.06.11, Figure 3.06.5).
Figure 3.06.5: Age-standardised proportion of hospitalisations (excluding dialysis) where a procedure was recorded, by Indigenous status, 2011–12 to 2020–21
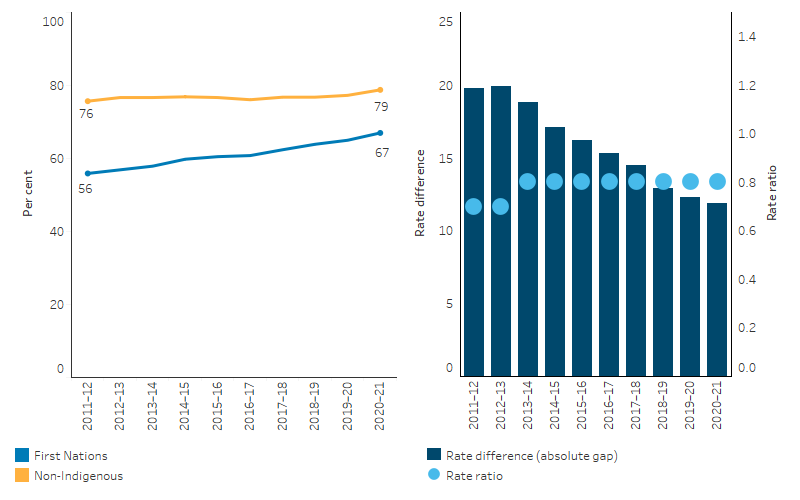
Source: Table D3.06.11. AIHW analysis of National Hospital Morbidity Database and ABS population estimates and projections (ABS 2019a, 2019b, 2022a, 2022b) for calculation of rates.
Considering hospitalised events for acute coronary syndrome, the age-standardised proportion that included either a coronary angiography or a definitive revascularisation procedure among First Nations adults increased by 15 percentage points between 2010–11 and 2019–20 (49% to 64%), with a similarly sized increase of 16 percentage points (57% to 73%) for non-Indigenous adults (AIHW 2023b). There was no apparent trend in the gap (rate difference), fluctuating between 5 and 16 percentage points over this period. There was also no apparent trend in the rate ratio (ranging between 0.8 and 0.9) (Figure 3.06.6).
Figure 3.06.6: Proportion of hospitalisations among adults for acute coronary syndrome events where the patient received a coronary angiography and/or a definitive revascularisation procedure, by Indigenous status, 2010–11 to 2019–20
Source: Better Cardiac Care measures for Aboriginal and Torres Strait Islander people: seventh national report 2022 (AIHW 2023b) – Data Table 3.3e.
Research and evaluation findings
A discussion paper examined the profound effects of colonialism on the healthcare access of indigenous peoples, particularly focusing on New Zealand’s Māori and Australia’s First Nations communities. The paper argues that colonial processes, including land dispossession, acculturation, social marginalisation, and political oppression, have directly impacted the health status of these indigenous groups. Such historical and ongoing inequalities manifest in higher rates of morbidity, mortality, and poorer health service utilisation among indigenous peoples. The discussion highlights key barriers to healthcare access for these communities, including socioeconomic factors, racial discrimination, and institutional racism. The study emphasises the intergenerational effects of colonisation, suggesting that the trauma and marginalisation experienced by indigenous peoples continue to affect their health and wellbeing. The authors conclude that recognising and addressing the historical and ongoing impacts of colonisation is crucial to improving healthcare access and outcomes for indigenous populations. They advocate for the inclusion of indigenous perspectives in healthcare reform and emphasise the need for culturally informed research and healthcare practices to address these deep-rooted disparities (Zambas & Wright 2016).
A review of qualitative studies was conducted on the hospital care experiences of indigenous patients. The review incorporated 21 primary studies from various countries, including Australia, Canada, New Zealand, and Kenya, covering a period from 2000 to 2016. The main aim of the study was to explore and understand the experiences and perceptions of indigenous people during hospitalisation for acute care. The key themes that emerged from this review were: strangers in a strange land; encountering dysfunctional interactions; and suffering stereotyping and assumptions. These themes underscore the sense of cultural alienation and marginalisation indigenous patients often feel in hospital settings. The review found that indigenous patients faced significant communication challenges due to language barriers and cultural differences, felt isolated due to being away from their community, and often had negative encounters with healthcare staff, characterised by superficial mechanistic relationships. They also experienced stereotyping and assumptions based on their indigenous status, which further negatively impacted their hospital experience. The review highlights that the hospital experiences of indigenous patients can significantly fall short of their expectations and needs. It is common for indigenous peoples to experience clinical encounters that still carry elements of discriminatory practices. Additionally, hospital policies may contribute to a discriminatory culture by not reflecting indigenous views. It is therefore unsurprising that they continue to avoid access to health services, even when they are required and are available. The review emphasises the importance of healthcare professionals being aware of these discrepancies and implementing strategies that allow for inclusive and individualised care. The findings call for a deep understanding and integration of cultural sensitivity in healthcare settings to improve the experiences and outcomes for indigenous patients (Mbuzi et al. 2017).
Research into addressing surgical inequity for First Nations people across the Australian health care system explored the barriers and disparities that exist in accessing care at 5 care points along the surgical journey: perception of need; access to primary care; access to specialist services; access to elective surgery; and surgical outcomes. At all care points, challenges were identified including: the different conceptions of health and health needs between First Nations clients (having a more holistic perspective, not prioritising non-urgent symptoms and delaying seeking care) and of health professionals (having a Western biomedical approach which does not incorporate an understanding of First Nations values and beliefs); lack of culturally secure care (existence of racism, mistrust, poor communication, lack of culturally appropriate referral pathways); lower access to specialist services (geographic barriers, unaffordable or lack of private health insurance, lack of First Nations specialists); less access to elective surgery (clinician bias, preoperative risk factors, long wait times); and poorer surgical outcomes (as a result of presentation at more advanced stages of disease, presence of comorbidities – but more research in understanding surgical outcomes is needed). Identifying and addressing the social determinants of health and discrimination along the pathway to surgical care are suggested as key to delivering more culturally secure models of care (O'Brien et al. 2021).
The burden of osteoarthritis disproportionately impacts First Nations people. First Nations men had approximately one-third the number of hip replacements that would have been expected compared with non-Indigenous men of the same age, while this number was one-fifth for First Nations women. Total knee replacements were also accessed at approximately one-half the expected rate based on incidence. This indicates that the uptake of total joint replacement (TJR) by First Nations people over the past 15 years is likely to have remained low. First Nations people undergoing TJR were significantly younger than non-Indigenous people suggesting that First Nations people experience a greater burden of osteoarthritis at an earlier age. A ‘treatment gap’ exists, whereby First Nations people are less likely to be offered surgical interventions as a treatment option. Further investigation is needed to understand whether low utilisation of TJR is a reflection of differences in healthcare access, including socioeconomic circumstances and access to private health insurance, systematic or decision-making biases and/or beliefs and knowledge about osteoarthritis and TJR among First Nations people, or a combination of these factors (O'Brien P. et al. 2022).
An expert panel undertook a comprehensive review into the hurdles, service gaps and practical challenges faced by First Nations patients receiving treatment for kidney disease (The Transplantation Society of Australia and New Zealand 2019). The review report, released in 2019, identified measures to address gaps in waitlisting and long-term transplant outcomes and improving First Nations dialysis patients’ health to improve their capacity to be waitlisted. Following the review, a National Indigenous Kidney Transplantation Taskforce (NIKTT) was established to implement and evaluate the recommendations from the review (further information is below in the Implications section).
A national study of ANZDATA Registry data from 2006–2016 found that First Nations patients were less likely than non-Indigenous patients to be added to the kidney transplantation waiting list during the first year of renal replacement therapy (Khanal et al. 2018). This disparity was not explained by differences in patient- or disease-related factors with the disparity more pronounced in the first year of renal replacement therapy and among older patients from remote regions. After initial listing, the likelihood of transplantation was higher in the first year and similar for both First Nations and non-Indigenous patients, but significantly lower for First Nations patients in subsequent years (Khanal et al. 2018).
A study conducted in 2005–06 found that treating specialists commonly identified First Nations patients as ‘non-compliers’ with their dialysis regimes and as high-risk kidney transplant candidates, but that this assessment was not systematic or formal (Anderson et al. 2012). There was variation in how specialists weighted these assessments in their decision making and uncertainty about the value of compliance status in predicting post-transplant outcomes. In Victoria, a patient study found that medical comorbidities were the main barrier to kidney transplant listing, but once listed, First Nations patients had a short waiting time due to accumulated ‘waiting time’ which begins when patients start dialysis (Atkinson & Goodman 2018). International research has found that patient aversion to transplantation (for cultural, social, religious, health or other reasons) may contribute to differential access by particular groups, but a study of First Nations patients in all states and territories, apart from Victoria and Tasmania, found they had a high level of interest in kidney transplantation (Devitt et al. 2017). However, patients experienced multiple communication barriers and felt that they and their families were poorly informed and disempowered about transplantation as an option. While patients needed to navigate cultural and social sensitivities, this did not seem to be a factor in patients’ decision-making. A study in Western Australia found that First Nations kidney recipients experienced poorer outcomes than non-Indigenous recipients and recommended future research be done into factors associated with better outcomes for First Nations recipients of kidney transplants (Howson et al. 2019).
A retrospective analysis conducted at the Central Australian Renal Service, Alice Springs, Australia, between January 2017 and June 2018, examined the barriers to timely waitlisting for kidney transplantation for First Nations people in Central Australia. It focused on 25 patients (20 First Nations and 5 non-Indigenous) on the kidney transplant waitlist to identify the reasons for delays in waitlisting, particularly among First Nations people. The primary aim was to compare the time taken for First Nations and non-Indigenous patients to complete the transplant assessment and be placed on the waitlist. The analysis found that First Nations people faced significantly longer wait times for kidney transplantation after starting dialysis – median 1,215 days for First Nations patients compared with 264 days for non-Indigenous patients. Delays were noted in starting the transplant assessment process and completing various assessment components, such as dental assessment, tissue typing, and reviews by transplant nephrologists and surgeons. Key factors contributing to delays for First Nations patients included systemic delays in the assessment, screening and clearance process (such as for cardiac, malignancy, respiratory and dental issues), and delays in investigations or clinical reviews which in turn compound the delay with other assessments needing to be redone as the process spreads out over time. The analysis highlighted in particular the need for more efficient cardiac assessments and interventions, especially in remote settings, and for optimising health systems to better cater to the needs of patients from diverse cultural and sociodemographic backgrounds. This approach could potentially reduce workup times and improve access to kidney transplantation for First Nations people (Tiong et al. 2022).
A study of patients admitted to Queensland hospitals for acute myocardial infarction (that is, heart attack) between 1998 and 2002 found that the rate of coronary procedures among First Nations patients was 22% lower than the rate for other patients (Coory & Walsh 2005). A more recent study in South Australia found that First Nations patients were less likely to receive a coronary angiography after controlling for age, comorbidities and remoteness (Tavella et al. 2016).
Research using data from the National Eye Health Survey 2015–16 found that the cataract surgery coverage rate is significantly lower among First Nations people than non-Indigenous Australians (Foreman et al. 2017). While First Nations children have a lower incidence of poor vision than other Australian children, the prevalence of vision impairment increases markedly with age: First Nations people over the age of 40 have nearly 3 times the rate of vision loss of other Australians (Foreman et al. 2017). There is evidence, however, of some improvement in recent years, with findings of the 2016 National Eye Health Survey (NEHS) indicating that the prevalence of blindness among First Nations adults has declined, possibly related to improvements in prevention and treatment services (AIHW 2023a). Most of the blindness and vision impairment experienced by First Nations people is caused by conditions that are preventable or amenable to treatment, that is, vision loss due to refractive error, cataract and diabetic retinopathy. For example, use of glasses (spectacles) and cataract surgery are two relatively low-cost effective interventions for treating the main causes of vision loss (Foreman et al. 2016). In the report Eye health measures for Aboriginal and Torres Strait Islander people 2023 (AIHW 2023b) it was shown that from 2013–14 to 2020–21, the age-standardised rate for cataract surgery for First Nations people increased from 6,462 to 8,691 per 1,000,000 but the rate was about 3% lower than the rate for non-Indigenous Australians (8,944 per 1,000,000). The median waiting time for elective cataract surgery for First Nations people was the same as that for non-Indigenous Australians (167 days).
First Nations children have some of the highest rates of otitis media (inflammation and infection of the middle ear) in the world. Prevention, early detection and treatment of otitis media for infant and children are critical to prevent associated hearing loss which impacts across the life course including poor language development and social skills, and educational disadvantage. First Nations children were 10 times more likely to be hospitalised for otitis media than non-Indigenous children but less likely to have in-hospital tympanostomy tube insertion (TTI) procedures. The median age of otitis media hospitalisation was 3 months younger among First Nations than non-Indigenous children. However, the median age of first TTI admission was 18 months older which indicates a delayed detection and treatment causing more serious adverse health outcomes (Westphal et al. 2019).
Analysis of 2016–17 hospitalisations for colonoscopy found that there was greater use of colonoscopy in areas with higher socioeconomic status, which have a low incidence of bowel cancer and low death rates, compared with areas of low socioeconomic status, which have the highest incidence and death rates (ACSQHC 2018). The rate of hospitalisations for colonoscopy for First Nations people was 47% lower than the rate for other Australians.
A whole-of-population data linkage study conducted in Queensland, covering individuals diagnosed with cancer between July 2011 and June 2012 aimed to quantify the direct out-of-pocket patient co-payments and time opportunity costs (length of hospital stay) incurred by First Nations people and non-Indigenous Australians diagnosed with cancer during the first-year post-diagnosis. Based on a census of 25,553 cancer patients, the study found that after adjusting for various factors, First Nations people accrued significantly less in post-diagnosis patient co-payments at 0–6 months (61% less) and 7–12 months (63% less) compared to non-Indigenous Australians. They also had significantly fewer post-diagnosis hospitalisations at 0–6 months (21% fewer) and 7–12 months (27% fewer). The study highlights the growing concern about the financial burden of cancer on patients. The financial impact and the time away from family and community due to hospital stays may affect a person’s decision to undertake or continue treatment. This research is significant as it identifies the financial cost of co-payments for First Nations people with cancer, as well as the number and length of hospitalisations as drivers of time opportunity costs. The study underlines the importance of considering both the direct financial costs and the time opportunity costs of cancer care, particularly for First Nations patients who may face unique challenges due to their socioeconomic and geographical circumstances. The study identifies that programs such as the Medicare Safety Net and Closing the Gap (CTG) PBS Co-payment Program may be effective in reducing the financial burden on First Nations patients, but further research is needed to fully understand the broader impacts of cancer-related costs (Callander et al. 2019).
The Lighthouse Hospital Project Phase 3, funded by the Australian Government Department of Health and led by the Heart Foundation and the Australian Hospital and Healthcare Association (AHHA), was a 3-year initiative from January 2017 to December 2019 (Heart Foundation 2022). It aimed to improve health outcomes for First Nations people with Acute Coronary Syndrome across 18 participating hospitals in Australia. These populations are significantly more likely to be admitted to hospital for heart-related issues, and experience higher rates of discharge against medical advice (DAMA). The project focused on reducing the incidence and impact of DAMA for these patients. Hospitals implemented continuous quality improvement projects using the Lighthouse hospital toolkit, which includes activities in 4 domains: governance, cultural competence, workforce, and care pathways. The evaluation utilised a mixed-methods design, integrating qualitative and quantitative data, including reviews of action plans, interviews with stakeholders, patient experience surveys, and hospital record data. The evaluation found the project strengthened relationships between hospital staff and community organisations, and improved care delivery tailored to the needs of First Nations patients. However, it was challenging to determine improvements in clinical procedures and treatments conclusively. Hospitals participating in the project provided better access to coronary procedures for First Nations patients with Acute Coronary Syndrome compared with national levels, but it was not clear that this was a result of the program, with no clear upward trend. There were potentially other factors at these participating hospitals that contributed to the higher rates of procedures. While most patients rated their hospital experience positively, the project did not significantly reduce DAMA rates during the implementation period. The study concluded that while progress was evident in various aspects, a longer timeframe, possibly 5–10 years, might be needed to realise the desired outcomes fully. The complexity of hospital settings and the need to navigate various challenges, including institutional racism and bureaucracy, were noted as factors impacting the project’s progress. The evaluation highlighted the importance of strong leadership, support, and a culturally safe workforce in implementing such initiatives (Heart Foundation 2022).
Implications
There is a clear disparity in accessibility and outcomes for hospital procedures between First Nations people and non-Indigenous Australians. This is seen across age, remoteness, jurisdiction and principal diagnosis. This measure has provided a few examples of the disparity within particular disease types, but the hospitalisation data and the use of principal diagnosis chapters is somewhat limited for a full analysis of this complex issue. Academic research can and does provide a deeper exploration of these disparities and the key drivers, as well as providing insight into how hospital services can improve.
A culturally safe and responsive primary health care system is also a prerequisite for effective hospital and specialist services for First Nations people. Several studies have found that improving patient-provider communication and collaboration makes it easier for people to navigate, understand and use information and services to take care of their health. This could include matching information to the patient’s needs and abilities, recognising the importance of asking questions, shared decision-making, and providing a range of avenues for communication (Hernandez et al. 2013; Øvretveit 2012). Aboriginal Health Workers and Liaison Officers (AHWLOs) are a unique workforce introduced to increase access to culturally safe care and, ultimately, help to address health inequities experienced by First Nations people. AHWLOs may improve communication between patients and medical staff, improve continuity of care and reduce patient discharge against medical advice (Mackean et al. 2020) (see measure 3.09 Self-discharge from hospital).
A significant body of work over the past 2 decades has sought to raise awareness and embed concepts of cultural respect in the Australian health system that are fundamental to improving access to quality and effective health care, and improving health outcomes for First Nations people. There has been a longstanding commitment by Australian governments to enable this.
The Cultural Respect Framework for Aboriginal and Torres Strait Islander Health 2016–2026: A national approach to building a culturally respectful health system plays a crucial role in reaffirming this commitment and provides a nationally consistent approach (AHMAC 2016). The Aboriginal and Torres Strait Islander Health Performance Framework plays a role in monitoring the commitment to embed cultural respect principles into the Australian health system.
Monitoring is also supported by the Cultural Safety in Health Care for Indigenous Australians: Monitoring Framework which covers 3 modules: culturally respectful health care services, patient experience of health care, and access to health care services. However, monitoring is limited by a lack of national and state-level data, particularly on the policies and practices of mainstream health services such as hospitals and the experiences of First Nations patients in hospitals (AIHW 2022a).
While there has been an increase in the proportion of First Nations people who received a hospital procedure and a decrease in the gap between the proportion of First Nations people and non-Indigenous Australians receiving a hospital procedure, a wide gap remains. In addition, the age-standardised proportion of hospitalisations for First Nations people that ended in discharge at own risk – an indirect measure of cultural safety in hospitals – decreased from 4.6% to 3.8% from 2011–12 to 2020–21 (see measure 3.09 Self-discharge from hospital).
The Ways of Thinking and Ways of Doing program was developed to ‘translate the systemic, organisational, and clinical elements of the Cultural Respect Framework into routine clinical practice’ (Liaw et al. 2019). A study of the effect of this program in Melbourne and Sydney general practice settings found that it did not significantly influence the First Nations health check rate or cultural respect levels. The authors suggested that cultural respect programs may require more than 12 months to have a positive effect.
As a result of historic and systemic factors, socioeconomic disparities can impact outcomes. The vast majority of hospital procedures for First Nations people are done in the public hospital system, whereas a much greater share of procedures for non-Indigenous Australians is done in the private hospital system. Low incomes and low take-up of private health insurance are likely having an effect. In the 2021 Census, 35% of First Nations adults were living in households in the bottom 20% of Australian incomes. In the 2018–19 National Aboriginal and Torres Strait Islander Health Survey, 21% of First Nations people in Non-remote areas reported they had private health insurance. The lower proportion of procedures per hospitalisation is likely to be associated with private health insurance coverage and lower access to private hospitals. This may influence the rate of preventative hospital treatments. Research has found that, after adjusting for other factors, the strongest association with coronary angiography rates was admissions to private hospitals (Chew et al. 2016). This also highlights the inequitable access to specialist care for many First Nations people that are largely reliant on the public hospital system.
First Nations patients with chronic disease sometimes present later in the course of these illnesses, compared with non-Indigenous Australians, which affects treatment options (Valery et al. 2006). Other factors that have been suggested include that the presence of comorbidities limits treatment options (although this does not explain the difference in coronary procedures outlined above); clinical judgments concerning post-procedural compliance; communication issues, such as for patients whose main language is not English; and patient knowledge and attitudes, for example, fatalistic attitudes towards cancer. Physical, social and cultural distance from health services also play a role, along with financial issues patients and their families may face when seeking treatment in specialist referral services (Miller et al. 2010; Shahid et al. 2009). An analysis of 2017–18 Medicare data shows that the rate of claims for specialist services for First Nations people was below non-Indigenous Australians for both in and out-of-hospital care (Table D3.14.23). Effective strategies will require a better understanding of the factors leading to the observed disparities.
In May 2023, the Australian Government committed over $500 million to reduce the burden of lung cancer in Australia and drive equitable cancer outcomes for First Nations people. Co-designed with First Nations people, the program will maximise prevention and early detection of lung cancer and aims to achieve equity in cancer outcomes for vulnerable groups. $238.5 million was committed to support achieving equity in overall cancer outcomes for First Nations people. This investment will build the capacity and capability of the Aboriginal Community Controlled Health Services sector to support cancer care needs on the ground, tailored to local need and priorities; and ensure mainstream cancer care services are culturally safe and accessible to First Nations people (Cancer Australia 2023).
In 2018, cardiovascular disease was the second leading contributor to the gap in disease burden between First Nations people and non-Indigenous Australians (AIHW 2021b). The National Recommendations for Better Cardiac Care for Aboriginal and Torres Strait Islander People (see measure 1.05 Cardiovascular disease) aim to address the disparities in cardiovascular care. The Lighthouse Hospital Project has found that some key initiatives have led to improvements in care such as the expansion of the Aboriginal Health Workforce, better Indigenous status identification of patients, engaging in effective partnerships with First Nations communities, fostering champions among clinical staff, patient-centred care and improved communication (Australian Healthcare & Hospitals Association 2021).
The survival rate of First Nations people with end-stage kidney disease that require renal replacement therapy has significantly increased and evidence suggests the survival gap has closed between First Nations and non-Indigenous patients (Lawton et al. 2015). However, there remain disparities and barriers for First Nations people accessing kidney transplantation. Qualitative research has unpacked some of these barriers and their experiences of the health system on the treatment pathway, including information needs, distance and the effect of being away from home (Cass et al. 2003). For the health system to be more effective in delivering transplantation services to First Nations people in Australia, it requires an understanding of their needs and motivations in seeking kidney transplantation (Cass et al. 2003). Other studies explored above highlighted a range of systemic barriers to First Nations people accessing kidney transplantation (Anderson et al. 2012; Khanal et al. 2018; Tiong et al. 2022) which require system level responses.
The 2019 Review into kidney transplantation by the Transplantation Society of Australia and New Zealand explored the complex challenges associated with delivering appropriate kidney health services in remote areas. The review examined the burden of comorbidities affecting suitability for transplantation, waiting lists, the dislocation from moving to transplant centres and the high rates of post-transplant complications. It made 35 recommendations aimed at improving health services requiring close collaboration between consumers, academia, health services, peak bodies and governments. The review also illustrated the systemic biases in the kidney transplant system and identified potential mitigation strategies (Cass Alan 2019; The Transplantation Society of Australia and New Zealand 2019). A National Indigenous Kidney Transplantation Taskforce (NIKTT) was established to implement and evaluate the recommendations from the review.
A scoping review by the NIKTT identified 4 key domains of action (each with several recommendations) to address cultural bias in kidney transplantation for First Nations people: Inclusion of First Nations people; Workforce; Service delivery approach and models of care; and Structures and policies (Kelly et al. 2019). The review emphasises the importance of co-designed and co-created participative approaches to research, implementation and evaluation for the development of new models of transplantation care for First Nations people living with kidney disease (Lowitja Institute 2020).
The National Aboriginal and Torres Strait Islander Health Plan (the Health Plan), released in December 2021, is the overarching policy for First Nations’ health and health care in Australia. It recognises early access to culturally safe and responsive primary care is key to addressing the higher hospitalisation rates of First Nations people, where presentation often occurs at a later stage of disease and can lead to higher rates of death. The Health Plan emphasises that action to address cardiovascular disease, diabetes, ear, eye and renal health, and rheumatic heart disease, remain key priorities. Lessons learned from the work to improve the health system in delivering cardiac care and kidney transplantation may also help address other disparities in hospital services for First Nations people.
The Health Plan prioritises making acute care settings accessible, culturally safe and responsive to address gaps between experiences of First Nations people and non-Indigenous Australians in hospitals. These include addressing the gap in surgery procedures and wait times, and in the rates of early discharge or discharge against medical advice. This will require hospitals to implement strategies to better deliver holistic, coordinated and culturally safe models of care including harnessing traditional health workers to provide complementary care, and establishing coordination pathways with Aboriginal Community Controlled Health Services. Addressing these disparities requires working with communities to understand their needs and addressing the systemic factors that result in poorer hospital outcomes. Some of these systemic factors have been outlined in this measure and impact upon First Nations people receiving equitable access to hospital procedures. The Health Plan has also made identifying and eliminating racism in mainstream health settings a key priority. It seeks to achieve this by prioritising patient experiences and improving cultural safety. This is supported by training, enhanced data collection, reporting and accountability.
The policy context is at Policies and strategies.
References
- ABS (Australian Bureau of Statistics) 2019a. Estimates and Projections, Aboriginal and Torres Strait Islander Australians, 2006 - 2031. Canberra, Australia: Australian Bureau of Statistics.
- ABS 2019b. Estimates and Projections, Aboriginal and Torres Strait Islander Australians. Canberra, Australia: Australian Bureau of Statistics.
- ABS 2022a. National, state and territory population, March 2022. Canberra, Australia: Australian Bureau of Statistics.
- ABS 2022b. National, state and territory population, Reference Period December 2022. Canberra, Australia: Australian Bureau of Statistics.
- ABS & AIHW (Australian Institute of Health and Welfare) 2008. The health and welfare of Australia's Aboriginal and Torres Strait Islander peoples 2008. Canberra: ABS & AIHW.
- ACSQHC (Australian Commission On Safety And Quality In Health Care) 2018. Third Australian Atlas of Healthcare Variation. Sydney.
- AHMAC (Australian Health Ministers' Advisory Council) 2016. Cultural Respect Framework 2016-2026 for Aboriginal and Torres Strait Islander health. Canberra: AHMAC.
- AIHW (Australian Institute of Health and Welfare) 2021a. Better Cardiac Care measures for Aboriginal and Torres Strait Islander people: sixth national report 2021. Canberra: AIHW.
- AIHW 2021b. Australian Burden of Disease Study 2018 – Key findings. Cat. no. BOD 28. Canberra: AIHW. Viewed 19 October.
- AIHW 2021c. Admitted patient care 2018-19 3: Who used these services? . Canberra: AIHW
- AIHW 2022a. Cultural safety in health care for Indigenous Australians: monitoring framework. Canberra.
- AIHW 2022b. Admitted patient care 2020-21: 3 Who used admitted patient services? Canberra: AIHW. Viewed 18 October 2023.
- AIHW 2023a. Eye health measures for Aboriginal and Torres Strait Islander people 2022: in brief. Canberra: AIHW.
- AIHW 2023b. Better Cardiac Care measures for Aboriginal and Torres Strait Islander people: seventh national report 2022 (data update). Canberra: AIHW. Viewed 11 October 2023.
- Anderson K, Devitt J, Cunningham J, Preece C, Jardine M & Cass A 2012. If you can't comply with dialysis, how do you expect me to trust you with transplantation? Australian nephrologists' views on indigenous Australians' 'non-compliance' and their suitability for kidney transplantation. International Journal for Equity in Health 11:21.
- Atkinson A & Goodman D 2018. Overcoming barriers for Indigenous Australians gaining access to the kidney transplant waiting list. Renal Society of Australasia Journal 14:60-.
- Australian Healthcare & Hospitals Association 2021. The Lighthouse Hospital Project.
- Bourke CJ, Marrie H & Marrie A 2019. Transforming institutional racism at an Australian hospital. Australian Health Review 43:611-8.
- Callander E, Bates N, Lindsay D, Larkins S, Preston R, Topp SM et al. 2019. The patient co-payment and opportunity costs of accessing healthcare for Indigenous Australians with cancer: A whole of population data linkage study. Asia Pac J Clin Oncol 15:309-15.
- Cancer Australia 2023. Australian Government announces over $500 million to improve cancer outcomes for Australians. Cancer Australia, Australian Government.
- Cass A 2019. What the research says. The Transplantation Society of Australia and New Zealand.
- Cass A, Cunningham, J., Snelling, P., Wang, Z & Hoy, W. 2003. Renal transplantation for Indigenous Australians: identifying the barriers to equitable access, Ethnicity & Health, vol. 8, no. 2, pp. 111-119.
- Chew DP, MacIsaac AI, Lefkovits J, Harper RW, Slawomirski L, Braddock D et al. 2016. Variation in coronary angiography rates in Australia: correlations with socio-demographic, health service and disease burden indices. The Medical Journal of Australia 205:114-20.
- Condon JR, Cunningham J, Barnes T, Armstrong BK & Selva-Nayagam S 2006. Cancer diagnosis and treatment in the Northern Territory: assessing health service performance for Indigenous Australians. Internal Medicine Journal 36:498-505.
- Congress of Aboriginal and Torres Strait Islander Nurses and Midwives 2016. Cultural Safety in policy and practice seminar report: summary and implications. Canberra: CATSINaM.
- Coory MD & Walsh WF 2005. Rates of percutaneous coronary interventions and bypass surgery after acute myocardial infarction in Indigenous patients. The Medical Journal of Australia 182:507-12.
- Cunningham J 2002. Diagnostic and therapeutic procedures among Australian hospital patients identified as Indigenous. The Medical Journal of Australia 176:58-62.
- Devitt J, Anderson K, Cunningham J, Preece C, Snelling P & Cass A 2017. Difficult conversations: Australian Indigenous patients’ views on kidney transplantation. BMC nephrology 18:310.
- Foreman J, Keel S, Xie J, van Wijngaarden P, Crowston J, Taylor HR et al. 2016. National Eye Health Survey Melbourne: Vision 2020 and Centre for Eye Research Australia.
- Foreman J, Xie J, Keel S, Van Wijngaarden P, Crowston J, Taylor H et al. 2017. Cataract surgery coverage rates for Indigenous and non-Indigenous Australians: the National Eye Health Survey. Medical Journal of Australia 207:256-61.
- Hall SE, Bulsara CE, Bulsara MK, Leahy TG, Culbong MR, Hendrie D et al. 2004. Treatment patterns for cancer in Western Australia: does being Indigenous make a difference? The Medical Journal of Australia 181:191-4.
- Heart Foundation 2022. Lighthouse Hospital Project Phase 3 - Summary of evaluation findings. Heart Foundation.
- Henry BR, Houston S & Mooney G 2004. Institutional racism in Australian healthcare: a plea for decency. The Medical Journal of Australia 180:517-20.
- Hernandez SE, Conrad DA, Marcus-Smith MS, Reed P & Watts C 2013. Patient-centered innovation in health care organizations: a conceptual framework and case study application. Health Care Manage Rev 38:166-75.
- Howson P, Irish AB, D'Orsogna L, Chakera A, Swaminathan R, Perry G et al. 2019. Allograft and patient outcomes between Indigenous and non-Indigenous kidney transplant recipients. Transplantation.
- Kelly J, Dent P, Owen K, Schwartzkopff K & O'Donnell K 2019. Cultural bias Indigenous kidney care and kidney transplantation report.
- Khanal N, Lawton PD, Cass A & McDonald SP 2018. Disparity of access to kidney transplantation by Indigenous and non‐Indigenous Australians. The Medical Journal of Australia 209:261-6.
- Laverty M, McDermott DR & Calma T 2017. Embedding cultural safety in Australia’s main health care standards. The Medical Journal of Australia 207:15-6.
- Lawton PD, Cunningham J, Zhao Y, Gray NA, Chatfield MD, Baade PD et al. 2015. Survival of Indigenous Australians receiving renal replacement therapy: closing the gap? The Medical Journal of Australia 202:200-4.
- Liaw S-T, Wade V, Furler JS, Hasan I, Lau P, Kelaher M et al. 2019. Cultural respect in general practice: a cluster randomised controlled trial. Medical Journal of Australia 210:263-8.
- Lowitja Institute 2020. Cultural bias initiatives to improve kidney transplantation for Aboriginal and Torres Strait Islander people. Melbourne, Australia: Lowitja Institute.
- Mackean T, Withall E, Dwyer J & Wilson A 2020. Role of Aboriginal Health Workers and Liaison Officers in quality care in the Australian acute care setting: a systematic review. Australian Health Review 44:427-33.
- Malatzky C, Haines H & Glenister K 2020. Racism in a place of healthcare: The qualitative case of a rural Australian hospital. Journal of Community Medicine & Health Education 10: Article number: 1000681.
- Mbuzi V, Fulbrook P & Jessup M 2017. Indigenous peoples' experiences and perceptions of hospitalisation for acute care: A metasynthesis of qualitative studies. Int J Nurs Stud 71:39-49.
- Miller J, Knott V, Wilson C, Cunningham J, Condon J & Roder Dea 2010. Aboriginal and Torres Strait Islander Cancer Control Research Project. Sydney: Cancer Australia.
- O'Brien P, Bunzli S, Lin I, Bessarab D, Coffin J, Dowsey M et al. 2021. Addressing surgical inequity for Aboriginal and Torres Strait Islander people in Australia's universal health care system: a call to action. ANZ Journal of Surgery 91:238-44.
- O'Brien P, Thuraisingam S, Bunzli S, Lin I, Bessarab D, Coffin J et al. 2022. Total joint replacement may be a valuable treatment for Aboriginal and Torres Strait Islander people with osteoarthritis, but uptake is low. ANZ J Surg 92:2676-82.
- Øvretveit J 2012. Summary of 'Do changes to patient-provider relationships improve quality and save money?'. London: The Health Foundation.
- Shahid S, Finn L, Bessarab D & Thompson S 2009. Understanding, beliefs and perspectives of Aboriginal people in Western Australia about cancer and its impact on access to cancer services. BMC health services research 9:132.
- Tavella R, McBride K, Keech W, Kelly J, Rischbieth A, Zeitz C et al. 2016. Disparities in acute in-hospital cardiovascular care for Aboriginal and non-Aboriginal South Australians. The Medical Journal of Australia 205:222-7.
- The Transplantation Society of Australia and New Zealand 2019. Improving Access to and Outcomes of Kidney Transplantation for Aboriginal and Torres Strait Islander People in Australia: Performance Report.
- Tiong MK, Thomas S, Fernandes DK & Cherian S 2022. Examining barriers to timely waitlisting for kidney transplantation for Indigenous Australians in Central Australia. Internal Medicine Journal 52:288-94.
- Valery P, Coory M, Stirling J & Green AC 2006. Cancer diagnosis, treatment, and survival in Indigenous and non-Indigenous Australians: a matched cohort study. The Lancet 367:1842-8.
- Westphal DW, Lehmann D, Williams SA, Richmond PC, Lannigan FJ, Fathima P et al. 2019. Australian Aboriginal children have higher hospitalization rates for otitis media but lower surgical procedures than non-Aboriginal children: A record linkage population-based cohort study. PloS one 14.
- Zambas SI & Wright J 2016. Impact of colonialism on Māori and Aboriginal healthcare access: a discussion paper. Contemp Nurse 52:398-409.

