Key messages
- Cancer and other neoplasms were the leading broad cause of death for Indigenous Australians, accounting for 3,612 deaths (23% of total deaths), most of which were due to malignant neoplasms (3,563 deaths).
- The most common broad causes of death due to cancer for Indigenous Australians were cancers of the digestive organs at 30% (for example, liver cancer) and respiratory organs at 26% (for example, lung cancer).
- From 2010 to 2019, the age-standardised death rate due to cancer and other neoplasms increased by 12% for Indigenous Australians, while the rate for non-Indigenous Australians declined by 10%, resulting in a widening of the gap.
- In the 5-year period 2014–2018, there were 9,262 new cases of cancer among Aboriginal and Torres Strait Islander people. Lung cancer was the most common (1,404 cases or 15% of all new cases), followed by female breast cancer (1,150 or 12%), bowel cancer (850 or 9%) and prostate cancer (765 or 8%).
- For Indigenous males, cancer incidence rates were highest for prostate cancer (43 cases per 100,000 males), followed by lung cancer (41 per 100,000). For Indigenous females, incidence rates were highest for breast cancer (64 cases per 100,000 females), followed by lung cancer (37 per 100,000)
- Cancer incidence rates for Indigenous Australians were highest in Outer regional areas (281 per 100,000) and lowest in Very remote areas (221 per 100,000).
- In 2014–2018, the five-year crude survival rate for all cancers combined was lower for both Indigenous males (44%) and females (52%) than non-Indigenous males (58%) and females (63%).
- There were 11,970 hospitalisations for Indigenous Australians with a principal diagnosis of cancer between July 2017 and June 2019 – a rate of 7.2 hospitalisations per 1,000 population.
- Between 2009–10 and 2018–19, the age-standardised rate of hospitalisations with a principal diagnosis of cancer increased among Indigenous Australians (from 9.6 to 13 per 1,000) while it decreased among non-Indigenous Australians (from 17.3 to 16.0 per 1,000).
- For Indigenous males, the hospitalisation rates for prostate cancer increased by 31% between 2009–10 and 2018–19, while for Indigenous females hospitalisation rates of breast cancer increased by 16%.
- The gap between Indigenous and non-Indigenous Australians in death rates due to cancer was 2.5 times as high in remote areas as in non-remote areas (gap of 109 compared with 44 deaths per 100,000, respectively).
- The rate of disease burden due to cancer and other neoplasms for Indigenous Australians was 1.7 times the rate for non-Indigenous Australians in 2018 (50 and 30 DALY per 1,000 people, respectively). Cancer and other neoplasms was responsible for 9.1% of the total gap in burden of disease between Indigenous and non-Indigenous Australians.
- The joint effect of 19 selected behavioural, metabolic, environmental and dietary risk factors were found to have contributed 56% of the burden for cancer for Indigenous Australians in 2018, the biggest contributors being tobacco use (37%) and alcohol use (9.2%).
- Indigenous Australians have a higher incidence of fatal, screen-detectable and preventable cancers, and are more likely to be diagnosed at more advanced stages, often with comorbidities that are more complex.
- Evidence suggests that improvements in cancer care for Indigenous Australians are required, including in cancer diagnosis, treatment and health support services so they are more accessible and acceptable to Indigenous Australians.
Why is it important?
Cancer is a group of diseases in which abnormal cells proliferate and spread. These cells can form a malignant tumour that can invade and damage the surrounding area and spread (metastasise) to other parts of the body through the bloodstream or the lymphatic system. If the spread of these tumours is not controlled, it can cause death. The effectiveness of treatment and survival rates can vary between different cancers and patients (AIHW 2021).
While the causes of many cancers are not fully understood, there are some known risk factors, some of which may be modifiable and some which are not. These risk factors include biomedical factors (for example genetic susceptibility and hormonal factors), behavioural factors (for example smoking, alcohol consumption and physical inactivity) and environmental factors (for example sunlight and radiation) (AIHW 2019, 2021). Early diagnosis and access to culturally safe treatment are key to survival.
Aboriginal and Torres Strait Islander people have a higher incidence of fatal, screen-detectable and preventable cancers and are more likely to be diagnosed at more advanced stages, often with comorbidities that are more complex (Cunningham et al. 2008). For more on cancer screening, see measure 3.04 Early detection and early treatment. Compared with non-Indigenous Australians diagnosed with the same cancer, Indigenous Australians are disadvantaged because they are usually diagnosed later with more advanced disease, are less likely to have treatment, and often have to wait longer for surgery than non-Indigenous patients (Hall et al. 2004; Valery et al. 2006). This highlights the inequities within the health system experienced by Indigenous Australians.
The National Aboriginal and Torres Strait Islander Health Plan 2021-2031 (the Health Plan), released in December 2021, provides a strong overarching policy framework for Aboriginal and Torres Strait Islander health and wellbeing. ‘Priority Five’ of the Health Plan focuses on early intervention approaches that are accessible to Indigenous Australians and that provide timely, high quality, effective, culturally safe and responsive care. This includes an objective to deliver targeted action to improve cancer screening rates and care pathways for treatment including by addressing barriers to identifying, treating and managing cancer.
The Health Plan is discussed further in the Implications section of this measure.
Burden of disease
In 2018, cancer and other neoplasms accounted for 10% of the total disease burden among Indigenous Australians and was the fourth leading cause of burden for Indigenous males (9.8%) and the second leading cause for Indigenous females (10%).
Of the total burden due to cancer and other neoplasms among Indigenous Australians, 94% was due to premature death (fatal burden). Cancer and other neoplasms accounted for one-fifth (20%) of the total fatal burden for Indigenous Australians.
Lung (25%), mouth & pharyngeal (10%), bowel (8%) and liver (7%) cancers accounted for half (50%) of the burden due to cancer and other neoplasms among Indigenous Australians. These may be linked to smoking, risky alcohol consumption and higher levels of chronic infections. In 2018, 37% of the burden due to cancer among Indigenous Australians was attributed to tobacco use, and 9.2% to alcohol use.
After adjusting for differences in the age-structure between the two populations, the rate of burden due to cancer and other neoplasms for Indigenous Australians was 1.7 times the rate for non-Indigenous Australians (50 and 30 DALY per 1,000 people, respectively). Cancer and other neoplasms was responsible for 9.1% of the total gap between Indigenous and non-Indigenous Australians (AIHW 2022a).
Data findings
Cancer incidence
Data in this section are sourced from the Australian Cancer Database, with data for five jurisdictions combined for analysis: New South Wales, Victoria, Queensland, Western Australia and the Northern Territory. The data collected from these jurisdictions have higher level of coverage and reporting of Indigenous status and sufficient incidence counts to support analysis. Due to incomplete identification of Indigenous status in the data, the number of cancer incidence among Indigenous Australians and the true difference between Indigenous and non-Indigenous Australians are likely underestimated. Data for the other three jurisdictions are excluded because the Indigenous status variable was considered not of sufficient quality (see also Data sources and quality).
In the 5-year period 2014–2018 (based on calendar years), there were 9,262 new cases of cancer diagnosed among Indigenous Australians in the five jurisdictions combined for analysis. Lung cancer was the most common (1,404 cases, or 15% of all new cases), followed by female breast cancer (1,150 or 12%), bowel cancer (850 cases, 9%) and prostate cancer (765, 8%).
For all cancers combined, the cancer incidence rate among Indigenous Australians in 2014–2018 was 257 new cases of cancer per 100,000 population.
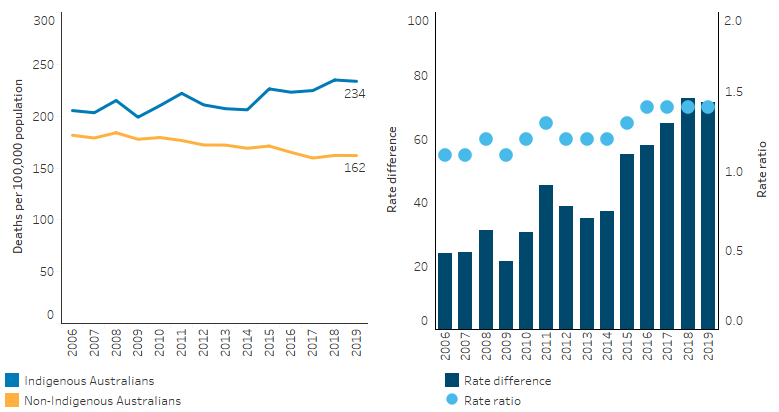
For Indigenous males, cancer incidence rates were highest for prostate cancer (43 cases per 100,000; 765 cases), followed by lung cancer (41 cases per 100,000; 733 cases). For Indigenous females, incidence rates were highest for breast cancer (64 per 100,000; 1,150 cases) followed by lung cancer (37 per 100,000; 671 cases) (Table D1.08.1, Figure 1.08.1).
Figure 1.08.1: Incidence of selected cancers among Indigenous Australians, by sex, NSW, Vic, Qld, WA and the NT combined, 2014–2018
Source: Table D1.08.1. AIHW analysis of Australian Cancer Database 2018.
By remoteness, cancer incidence rates for Indigenous Australians were highest in Outer regional and Remote areas (281 and 276 per 100,000, respectively), followed by Major cities and Inner regional areas (248 and 263 per 100,000, respectively) and were lowest in Very remote areas (221 per 100,000) (Table D1.08.20).
After adjusting for differences in the age-structure across remoteness areas, cancer incidence rates decreased with increasing remoteness. That is, rates were highest in Major cities (542 per 100,000) and lowest in Very remote areas (466 per 100,000).
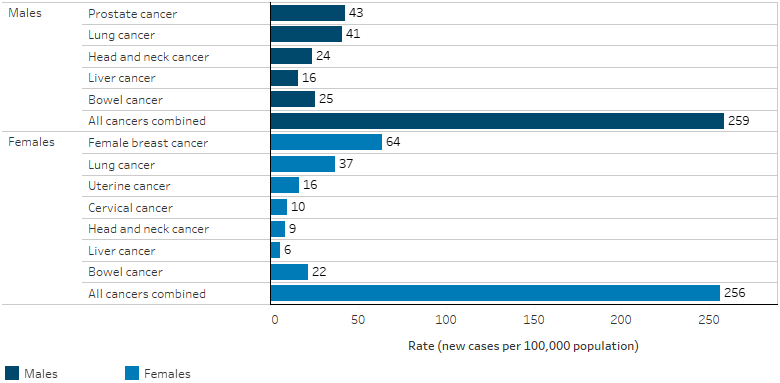
Cancer incidence rates increased with increasing age, from 49 cases per 100,000 for Indigenous Australians aged under 45, to 2,740 cases per 100,000 for those aged 75 and over (Figure 1.08.2).
Indigenous Australians aged under 45 had lower cancer incidence rates than non-Indigenous Australians (49 and 71 per 100,000 respectively). However, for those aged 45 and over, the cancer incidence rates were higher for Indigenous Australians (Table D1.08.2, Figure 1.08.2).
Figure 1.08.2: Age-specific cancer incidence rates, by Indigenous status, NSW, Vic, Qld, WA and the NT combined, 2014–2018
Source: Table D1.08.2. AIHW analysis of Australian Cancer Database 2018.
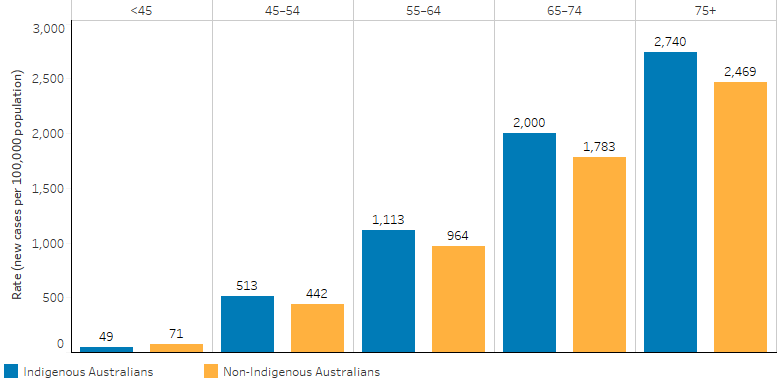
For Indigenous females, incidence rates for breast cancer were 12 per 100,000 for those aged under 45 and this increased with age to 428 per 100,000 for the age group 65–74, then decreased to 393 per 100,000 for those aged 75 and over. Breast cancer incidence rates were lower for Indigenous females than non-Indigenous females until age 64 and then this reversed from 65 and over.
For Indigenous males, incidence rates for prostate cancer were 0.5 per 100,000 for those aged under 45 and increased with age to a high of 648 per 100,000 for those aged 75 and over. Rates were lower for Indigenous males than non-Indigenous males across all age groups, however, the difference narrowed by the age group 75 and over (648 and 684 per 100,000, respectively).
For all Indigenous Australians, lung cancer incidence rates increased from 2.1 per 100,000 for those aged under 45, to 505 per 100,000 for those aged 75 and over. The rates were higher for Indigenous Australians than non-Indigenous Australians in all age groups, with rates 1.6–2.8 times the rate of non-Indigenous Australians (Table D1.08.2, Figure 1.08.3).
Figure 1.08.3: Age-specific incidence rates of selected cancers, by Indigenous status, NSW, Vic, Qld, WA and the NT combined, 2014–2018
Source: Table D1.08.2. AIHW analysis of Australian Cancer Database 2018.
In 2014–2018, after adjusting for differences in the age structure between the two populations, incidence rates for all cancers combined were 1.1 times as high for Indigenous Australians than non-Indigenous Australians, with an absolute difference of 58 cases per 100,000 population (Table D1.08.1).
The relative difference in cancer incidence rates varied by cancer type. In 2014–2018, incidence rates for Indigenous Australians were:
- 2.6 times as high as non-Indigenous Australians for liver cancer,
- 2.2 times as high for cervical cancer (females),
- 2.1 times as high for lung cancer,
- 1.9 times as high for head and neck cancer,
- 1.5 times as high for uterine cancer (females).
Indigenous Australians had a lower incidence rate than non-Indigenous Australians for bowel cancer (0.9 times as high), female breast cancer (0.9 times as high) and prostate cancer (males) (0.8 times as high) (Table D1.08.1).
Cancer survival rates
Data in this section are sourced from the Australian Cancer Database, with data for five jurisdictions pooled for analysis: New South Wales, Victoria, Queensland, Western Australia and the Northern Territory. Data for the other three jurisdictions is excluded because the Indigenous status variable was considered not of sufficient quality (see also Data sources and quality).
Crude survival is the proportion of cancer patients who are still alive a specified duration after their diagnosis, for example 1-year or 5-years. Cancer survival data do not distinguish between deaths from cancer deaths versus deaths from other causes. Therefore, survival rate could be affected by both cancer death rates and death rates from other causes. When comparing crude survival between Indigenous and non-Indigenous Australians it is not possible to say how much of the difference is due to differences in cancer outcomes versus other disease outcomes.
In 2014–2018, the 1-year crude survival rate for Indigenous Australians was 95% for female breast cancer, 94% for prostate cancer, 82% for bowel cancer, 70% for head and neck cancer and 38% for lung cancer. Indigenous females (74%) had a higher one-year crude survival rate for all cancers combined than Indigenous males (68%).
The 5-year crude survival rate for Indigenous Australians for 2014–2018 was 77% for female breast cancer, 77% for prostate cancer, 54% for bowel cancer, 42% for head and neck cancer and 11% for lung cancer. Indigenous females (52%) had a higher 5-year crude survival rate for all cancers combined than Indigenous males (44%).
In 2014–2018, the 5-year crude survival rate for all cancers combined was lower for both Indigenous males (44%) and females (52%) than non-Indigenous males (58%) and females (63%) (Table D1.08.8, Figure 1.08.4).
Figure 1.08.4: Five-year crude survival for selected cancers, by Indigenous status and sex, NSW, Vic, Qld, WA and the NT combined, 2014–2018
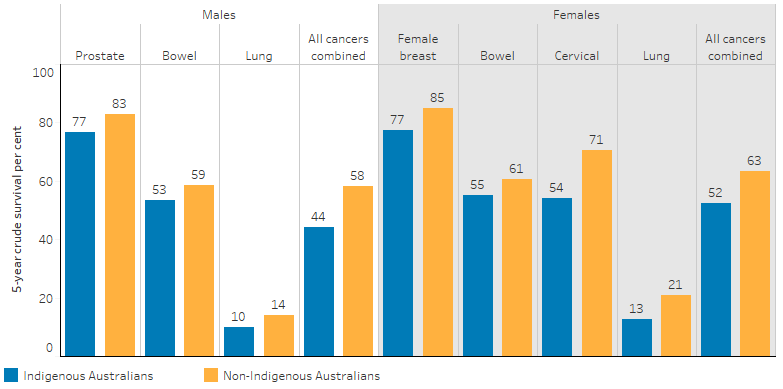
Source: Table D1.08.8. AIHW analysis of Australian Cancer Database 2018.
Deaths due to cancer
Deaths data in this section are from five jurisdictions for which the quality of Indigenous identification in the deaths data is considered to be adequate: namely, New South Wales, Queensland, Western Australia, South Australia and the Northern Territory. Data by remoteness are reported for all Australian states and territories combined (see Data sources: National Mortality Database).
Over the period 2015–2019, 3,612 Indigenous Australians died due to cancer and other neoplasms, and was the leading cause of death (accounting for 23.4% of all deaths of Indigenous Australians) (see measure 1.23 Leading causes of mortality) (Table D1.23.1).
The vast majority (99%, or 3,563) of these deaths were caused by cancer (that is, malignant neoplasms), corresponding to 23.1% of all deaths and a rate of 99 cancer deaths per 100,000 population.
For Indigenous Australians, the leading broad causes of cancer deaths were due to cancers of the: digestive organs (including liver cancer, 1,070 deaths or 30% of cancer and other neoplasm deaths); respiratory organs (including lungs, 935 deaths or 26%); lymphoid, haematopoietic and related tissue (259 deaths or 7.2%); ill-defined and unknown primary sites (250 deaths or 6.9%); and head and neck (216 deaths or 6%) (Table D1.23.5).
For Indigenous Australians the leading causes of death due to cancer varied by sex. There was a higher percentage of male deaths than female deaths attributable to cancers of digestive organs (32% of cancer and other neoplasm deaths compared with 27% for females) and cancers of the head and neck (8.2% of cancer and other neoplasm deaths compared with 3.4% for females). Breast cancer accounted for 11% of cancer and other neoplasm deaths among Indigenous females, and cancer of the female genital organs accounted for a further 10%. Prostate cancer accounted for 5.8% of cancer and other neoplasm deaths of Indigenous males (Table D1.23.12, Figure 1.08.5).
In 2015–2019, after adjusting for differences in the age structure between the two populations, Indigenous Australians died from cancer (malignant neoplasms) at 1.4 times the rate of non‑Indigenous Australians (226 and 162 per 100,000, respectively).
Figure 1.08.5: Proportion of cancer and other neoplasm deaths, Indigenous Australians, by cancer type and sex, NSW, Qld, WA, SA and the NT combined, 2015–2019
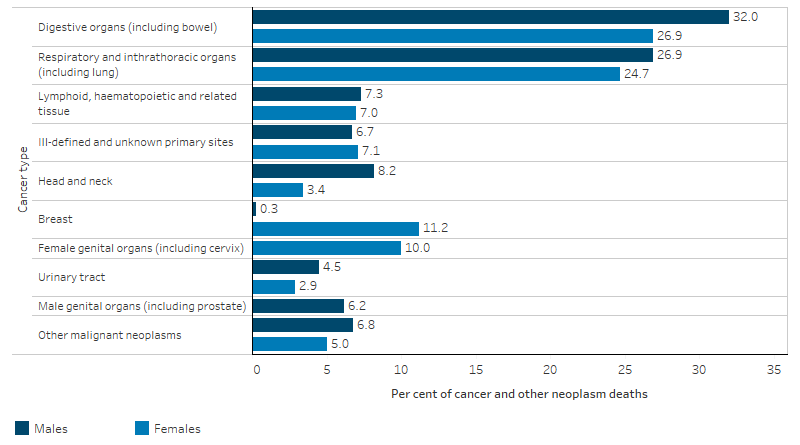
Source: Table D1.23.12. AIHW National Mortality Database.
Cancer and other neoplasms was the second leading cause of the gap in death rates between Indigenous and non-Indigenous Australians (18% of the total gap in death rates) (Table D1.23.1). The specific cancers contributing the most to this gap were cancers of the respiratory organs (45%) and cancers of the digestive system (33%) (Table D1.23.12).
In 2015–2019, for Indigenous Australians the crude death rate due to cancer and other neoplasms was the lowest in New South Wales (89 per 100,000) and highest in the Northern Territory (129 per 100,000) (Table D1.23.2). Across Australia, the rate was lower in non-remote areas (90 per 100,000) than in remote (126 per 100,000).
In remote areas, after adjusting for differences in the age structure between the two populations, the rate of death due to cancer among Indigenous Australians was 1.7 times the rate for non-Indigenous Australians (Table D1.23.30). The gap in death rates due to cancer between Indigenous and non-Indigenous Australians in remote areas was 2.5 times as high as the gap in non-remote areas (gap of 109 compared with 44 deaths per 100,000, respectively).
Cancer management
Based on the Bettering the Evaluation and Care of Health (2010–15) survey data, after adjusting for differences in the age structure between the two populations, the rate for cancer management by general practitioners (GPs) was lower for Indigenous Australians than for Other Australians (21 and 27 per 1,000 GP encounters, respectively) (Other Australians includes non-Indigenous Australians and those whose Indigenous status is unknown) (Table D1.08.10).
A body of work being undertaken by the National Aboriginal Community Controlled Health Organisation (NACCHO) aims to increase the number of eligible community members participating in the national bowel cancer screening program (NACCHO 2022). This builds on a successful pilot study conducted by the Menzies School of Health research and facilitates Aboriginal Community Controlled Health Organisations (ACCHOs) to distribute bowel cancer screening kits.
Hospitalisation due to cancer
Data in this section are sourced from the National Hospital Morbidity Database and are presented for the two financial years combined from July 2017 to June 2019.
Between July 2017 and June 2019, there were 11,970 hospitalisations with a principal diagnosis of cancer for Indigenous Australians, equivalent to rate of 7.2 hospitalisations per 1,000 population. Indigenous males had a higher hospitalisation rate than Indigenous females, at 7.9 and 6.5 per 1,000 population, respectively (Table D1.08.12).
After adjusting for differences in the age structure between the two populations, Indigenous Australians were hospitalised due to cancer at a rate of 13 hospitalisations per 1,000 population, lower than the rate for non-Indigenous Australians (16 per 1,000) (Table D1.08.11).
The hospitalisation rate for cancer as a principal diagnosis was lowest for Indigenous Australians living in the Northern Territory (5.5 hospitalisations per 1,000 population) and highest for those living in Victoria (9.7 per 1,000) (Table D1.08.12). Hospitalisation rates for cancer also varied by remoteness, with a lower rate among Indigenous Australians living in Very remote areas (5.8 per 1,000) compared with other remoteness areas (7.0 per 1,000 in Major cities, 7.5 per 1,000 in Inner regional areas, and 7.8 per 1,000 in both Outer regional and Remote areas) (Table D1.08.13).
The hospitalisation rate for Indigenous Australians for cancer as a principal diagnosis generally increased with age, except for those aged 0–4 (1.8 per 1,000), where the rates were higher than for those aged 5–14 and 15–24 (both 1.1 per 1,000). Hospitalisation rates were highest for Indigenous Australians aged 65 and over (51 per 1,000). The absolute difference in hospitalisation rates between Indigenous and non-Indigenous Australians was similar for those in all age groups under 45 years (ranging between 1.1 to 5.3), but was otherwise higher for non-Indigenous Australians.
Cancer is more likely to be recorded as an additional diagnosis than as the principal diagnosis in hospital data. Between July 2017 and June 2019, there were 30,928 hospitalisations for Indigenous Australians with either a principal or additional diagnosis of cancer – consisting of 11,970 with a principal diagnosis of cancer (including hospitalisations where cancer was both a principal and additional diagnosis of cancer), and a further 18,958 with an additional diagnosis of cancer.
For all hospitalisations for Indigenous Australians where cancer was recorded as a principal or additional diagnosis, 59% (18,104) were same-day hospitalisations and 41% (12,824) were overnight. The average length of stay for these hospitalisations was 3.9 days (Table D1.08.18).
Change over time
Data on cancer survival are sourced from the Australian Cancer Database. For the analysis, data are aggregated into 5-year groupings (based on calendar years) due to small counts in each individual year.
Over the period 1999–2003 to 2014–2018, both 1-year and 5-year crude survival rates increased across all the top 5 incident cancers for Indigenous Australians. Over this period, the 1-year crude survival rate for Indigenous Australians increased from 92% to 95% for female breast cancer, from 86% to 95% for prostate cancer, from 76% to 83% for bowel cancer, from 62% to 73% for head and neck cancers and from 25% to 40% for lung cancer.
The 5-year crude survival rate for Indigenous Australians increased from 71% to 78% for female breast cancer, from 55% to 79% for prostate cancer, from 47% to 56% for bowel cancer, and from 35% to 43% for head and neck cancers. For lung cancer, the 1-year survival rate increased from 10% in 2004–2008 to 12% in 2014–2018 (Table D1.08.16, Figure 1.08.6).
Figure 1.08.6: One-year and 5-year crude survival for selected cancers, Indigenous Australians, NSW, Vic, Qld, WA and the NT combined, 1999–2003 to 2014–2018
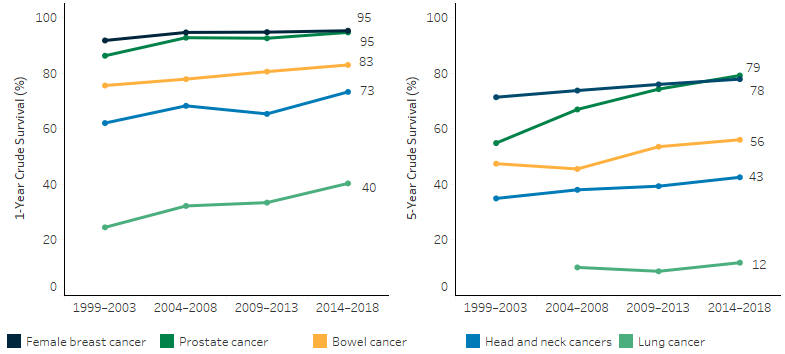
Notes:
1. Data shown for the top 5 incident cancers for Indigenous Australians.
2. Due to Australia’s ageing population the age distribution of the newly diagnosed cancer patient population is changing over time, with older people making up an increasing proportion. As older people tend to have lower survival than younger and middle-aged people, overall population survival in more recent time periods is not as high as it might otherwise have been. Consequently, apparent increases in survival over time shown in this graph may be underestimated.
Source: D1.08.16. AIHW analysis of Australian Cancer Database 2018.
Data on cancer mortality are sourced from the National Mortality Database. Trend information presented using calendar year data from 2006 to 2019, with a particular focus on the last decade from 2010 to 2019. Linear regression has been used to calculate the per cent change over time. This means that information from all years of the specified time period are used, rather than only the first and last points in the series (see Statistical terms and methods).
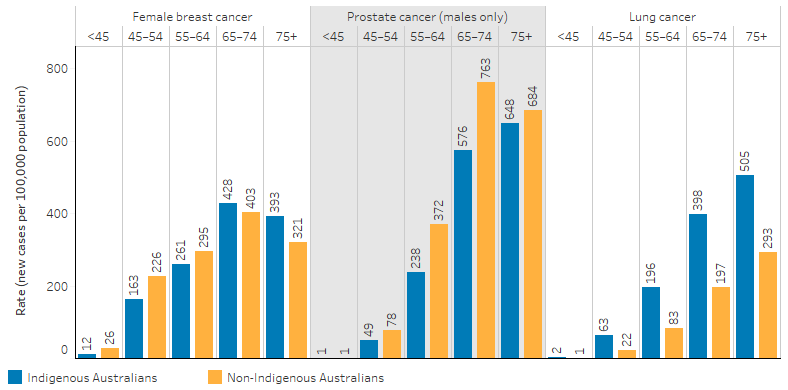
From 2006 to 2019, the rate of death due to cancer and other neoplasms increased by 14% for Indigenous Australians, while the rate for non‑Indigenous Australians declined by 13%, based on age-standardised rates. This resulted in the gap in cancer and other neoplasm deaths between the two populations widening over the period.
Over the decade from 2010 to 2019, the age-standardised rate of deaths due to cancer and other neoplasms for Indigenous Australians increased by 12%, while the rate for non-Indigenous Australians declined by 10%. The gap in the rates of the two populations widened over this period (Table D1.23.20, Figure 1.08.7).
Figure 1.08.7: Age-standardised death rates and changes in the gap due to cancer and other neoplasms, by Indigenous status, NSW, Qld, WA, SA and the NT combined, 2006 to 2019
Note: Rate difference is the age-standardised rate (per 100,000) for Indigenous Australians minus the age-standardised rate (per 100,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: Table D1.23.20. AIHW National Mortality Database.
Data on hospitalisations due to cancer are sourced from the National Hospital Morbidity Database, with trend information presented using financial year data from 2006–07 to 2018–19.
From 2006–07 to 2018–19, the age-standardised rate of hospitalisation due to cancer increased by 47% for Indigenous Australians (based on linear regression), while the rate for non‑Indigenous Australians declined by 6.7%.
Over the decade between 2009–10 and 2018–19, after adjusting for differences in the age structure between the two populations, there was a 47% increase in the hospitalisation rate for cancer among Indigenous Australians (from 9.6 to 13 hospitalisations per 1,000 population), in the six jurisdictions with Indigenous identification data of adequate quality (New South Wales, Victoria, Queensland, Western Australia, South Australia and the Northern Territory). The rate of hospitalisation due to cancer for non-Indigenous Australians decreased by 5.3% over the same period. Increases in the hospitalisation rate for Indigenous Australians coupled with the decreases for non-Indigenous Australians have resulted in in a narrowing of the gap over the period (Table D1.08.15, Figure 1.08.8).
Figure 1.08.8: Age-standardised hospitalisation rates and changes in the gap due to cancer and other neoplasms, by Indigenous status, NSW, Qld, WA, SA and the NT combined, 2006–07 to 2018–19
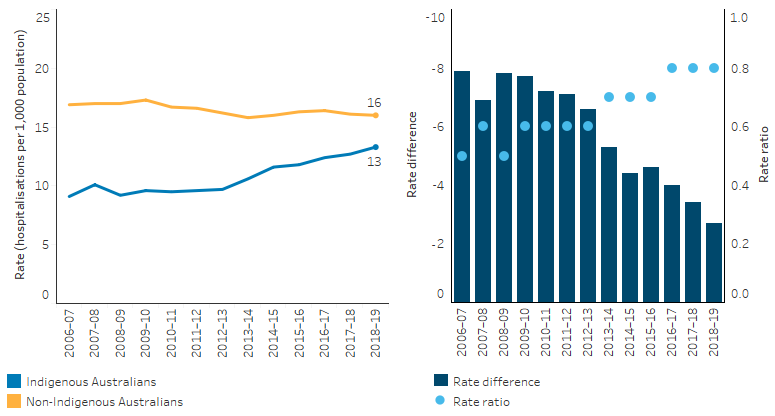
Note: Rate difference is the age-standardised rate (per 1,000) for Indigenous Australians minus the age-standardised rate (per 1,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: D1.08.15. AIHW analysis of National Hospital Morbidity Database.
Between 2009–10 and 2018–19, the age-standardised hospitalisation rates for the most common cancers for Indigenous Australians all increased:
- Bowel cancer hospitalisation rates increased by 52% (from an-age-standardised rate of 0.7 to 0.9 hospitalisations per 1,000 population).
- Lung cancer hospitalisation rates increased by 28% (from 1 per 1,000 to 1.4 per 1,000).
- Prostate cancer hospitalisation rates increased by 31% for Indigenous males (from 1.1 to 1.6 per 1,000).
- Breast cancer hospitalisation rates increased by 16% for Indigenous females (from 1.2 to 1.3 per 1,000) (Table D1.08.19).
Note that the per cent change over time data may appear inconsistent with the first and last rates in the series (provided in parentheses) due to the use of linear regression to calculate the per cent change (see Statistical terms and methods).
Research and evaluation findings
Cancer survival rates in Australia are among the highest in the world (OECD 2022). However, inequalities in cancer outcomes exist among Indigenous Australians and factors contributing to these disparities are complex and multifactorial. In 2020, the Cancer Council conducted a review of 48 papers to identify inequalities in cancer outcomes by Indigenous status. The review noted differences in cancer treatment reported by Indigenous Australians were associated with increased risk of death from breast, lung and colorectal cancer, which was influenced by the presence of comorbidities, more advanced stage at diagnosis, and less participation in diagnostic and treatment services (Bygrave et al. 2020). While these factors relate to accessibility of health services, the social, economic and cultural environments within which Indigenous Australians live and interact also influence cancer outcomes. These include personal beliefs, fears and attitudes about cancer, lower cancer symptom awareness, poorer health literacy, discrimination based on race or socioeconomic status, communication difficulties and geographic isolation (Bygrave et al. 2020).
A more recent literature review by Dasgupta et al. (2022) similarly found that the factors associated with cancer survival disparities by Indigenous status are multifactorial and complex. Factors found to explain some of the poorer cancer survival among Indigenous Australians included logistical, social, environmental, health system and cultural factors such as systemic discrimination, perceptions about cancer, communication barriers, lower health literacy and a lack of culturally appropriate care (Dasgupta et al. 2022).
The higher prevalence of cancer-related risk factors partly explains the patterns of Indigenous Australian cancer incidence and mortality (AIHW & Cancer Australia 2013). The Australian Burden of Disease Study 2018 found that the joint effect of 19 selected behavioural, metabolic, environmental and dietary risk factors contributed 56% of the burden for cancer for Indigenous Australians, the biggest contributors being tobacco use (37%) and alcohol use (9.2%) (AIHW 2022a) (see measure 2.15 Tobacco use). Understanding the drivers of these risk factors requires understanding of the broader socioeconomic determinants of health that impact upon Indigenous Australians for informing health interventions given the association between these determinants such as education, employment, income, and food insecurity with these risk factors. These are explored in more detail in Tier 2 Determinants of Health measures of this Health Performance Framework
Research on Indigenous Australian cancer outcomes also shows that other contributing factors include:
- having cancers that have a poor prognosis, such as lung cancer
- having fatal, screen-detectable cancers that are not detected
- being diagnosed with cancer at a later stage
- presenting with co-morbidities (that may lead to poorer outcomes)
- being less likely to receive any treatment, or adequate treatment (Cunningham et al. 2008; Jane et al. 2020; Moore et al. 2014; Valery et al. 2006).
A review by Haigh in 2018 provided a comprehensive synthesis of key information on cancer among Indigenous Australians. The review found that the factors contributing to poorer outcomes among Indigenous Australians diagnosed with cancer are complex. They reflect a broad range of historical, social and cultural determinants and the contribution of lifestyle and other health risk factors, combined with lower participation in screening programs, later diagnosis, lower uptake and completion of cancer treatment, and the presence of other chronic diseases. Providing effective cancer prevention and management also requires improved access to both high-quality primary health care services and tertiary specialist services. The review suggested that substantial improvements will also depend upon the effective implementation of more coordinated and comprehensive strategies that address the complex factors underlying the disadvantages experienced by Indigenous Australians, including action beyond the health service sector (Haigh et al. 2018).
A review into inequalities among Indigenous cancer patients showed an incidence of cancers with a poorer prognosis, such as lung cancer, is higher among Indigenous Australians, largely due to higher rates of smoking. It also found that wide disparities exist in cancer survival between Indigenous and non-Indigenous Australians, particularly in the first year after diagnosis. The review highlighted the need to improve cancer-related health services for Indigenous Australians; however, the available evidence is currently inadequate to effectively direct efforts. For example, despite the high cancer death rates, there is little information about the use of palliative care services by Indigenous Australians. The review noted the establishment and use of research collaborations such as DISCOVER-TT (the Centre for Research Excellence for Aboriginal and Torres Strait Islander Cancer Research), which provides an opportunity for developing targeted efforts in improving cancer outcomes for Indigenous Australians (Condon et al. 2013).
The DISCOVER-TT collaboration has since influenced other collaborations, policies and guidelines such as a pilot project to improve participation rates in Indigenous Australian bowel cancer screening and the National Aboriginal and Torres Strait Islander Cancer Framework. Another research collaboration is the Centre of Research Excellence in Targeted Approaches to Improve Cancer Services for Aboriginal and Torres Strait Islander Australians (TACTICS) that was established in 2019 and is focusing on emerging priorities and high-quality health services research.
Research suggests that survival rates among non-Indigenous patients are up to 50% greater than those for Indigenous patients within the first 12 months of diagnosis, but drops to a similar survival rate 2 years after diagnosis. However, 5-year survival was shown to be lower for Indigenous Australians compared with non-Indigenous Australians diagnosed with cancer (50.3% compared with 61.9%) (Cramb 2012). More recent data illustrated in Figure 1.08.4 also demonstrates a similar pattern and shows lower 5-year survival rates for Indigenous males (44%) and females (52%) compared with non-Indigenous males (58%) and females (63%) for all cancers combined.
While Indigenous Australian females are diagnosed with breast cancer at a lower rate than non-Indigenous females, they have a higher rate of death due to breast cancer than non-Indigenous Australian females (Tapia et al. 2017). Analysis found that the age-standardised death rate for Indigenous females was 1.2 times as high as for non-Indigenous females (AIHW 2018). Research also shows that Indigenous females are less likely to participate in breast screening and highly likely to feel culturally isolated in hospitals and clinics (Breast Cancer Network Australia 2018).
A study by Reath and Carey (2008) suggested that partnerships involving community members planning and implementing evidence-based strategies may improve the participation of Indigenous women in breast and cervical cancer screening. In the study, a female Indigenous worker and female GP developed and implemented local plans in three sites aimed at improving service coordination and access, GP knowledge, recall systems and health promotion with the objective of improving early detection of breast and cervical cancer in Indigenous women. An evaluation of the study identified the following success factors: collaboration between service providers; community participation in planning and delivery; an Indigenous health worker raising awareness among women and GPs; and a female GP providing a holistic service (Reath & Carey 2008).
For cervical cancer, studies show that later stage at diagnosis and availability of treatment, especially for females in remote areas, could be factors accounting for the higher cervical cancer death rates found for Indigenous females (Harvey et al. 2018). For more on cervical cancer screening see measure 3.04 Early detection and early treatment.
A study on cancer survival in children (aged 0–14) found that overall, 5-year survival was 75% for Indigenous children and 82% for non-Indigenous children. Following adjustments for remoteness of residence, socioeconomic disadvantage, cancer diagnostic group and year of diagnosis, Indigenous children had 1.36 times the risk of dying within 5 years of diagnosis compared with other children. The study noted that differences in place of residence, socioeconomic disadvantage, and cancer diagnostic group only partially explained the survival disadvantage of Indigenous children. The study also noted that other reasons underlying the disparities in childhood cancer outcomes by Indigenous status are yet to be determined and further research is required, but they may involve factors such as differences in timing and uptake of treatment (Valery et al. 2013).
Another study quantified hospital-recorded comorbidities using the Elixhauser Comorbidity Index to examine their influence on risk of cancer death and then considered effect variation by Indigenous status. The study found that comorbidities at diagnosis increased the risk of cancer death in addition to risks associated with Indigenous status, remoteness of residence and disease stage at diagnosis. The Indigenous cohort experienced comparatively greater exposure to comorbidities, which adds to disparities in cancer outcomes (Banham et al. 2018).
A matched cohort study was undertaken into cancer treatment and the risk of cancer death among Indigenous and non-Indigenous South Australians. The study quantified the influence of surgical, systemic and radiotherapy treatment on the risk of cancer death among matched cohorts of cancer cases and the comparative exposure of cohorts to these treatments. The study found that the effects of treatment did not differ between Indigenous and non-Indigenous cohorts. However, comparatively less exposure to surgical and systemic treatments among Indigenous cancer cases further complicated the disadvantages associated with geographic remoteness, advanced stage of disease and comorbid conditions at diagnosis and add to disparities in cancer deaths. System level responses to improving access, use and quality of effective treatments are needed to improve survival after cancer diagnosis (Banham et al. 2019).
Over the period 1998 to 2015, a study was conducted on cancer predictors among Indigenous adults from 26 rural and remote communities in Far North Queensland. The study showed Torres Strait Islanders have a significantly higher overall cancer incidence than Aboriginal people; diabetes was associated with a higher risk of cancer overall, particularly digestive system cancers; and smoking was a strong risk factor for cancer overall and particularly lung cancer. The study results indicated different cancer profiles for the Torres Strait Islander population (with higher rates of diabetes) and the Aboriginal population (with higher rates of smoking). These differences highlight the need for a customised mix of preventive strategies for these population groups (Li et al. 2018).
A cohort study into patterns of care and comorbidities among Indigenous and non-Indigenous cancer patients in Queensland showed that Indigenous Australians were diagnosed with more advanced cancer, had greater comorbidity, received less cancer treatment and were 30% more likely to die from cancer. The study found that survival was 60% lower for Indigenous Australians in the first year after diagnosis, but not significantly different in subsequent years. The 1‑year survival disparity was likely to be related to a lack of cancer treatment. However, the study also found that Indigenous Australians receiving cancer treatment had poorer outcomes overall, despite comparable time to commencement, duration and amount of treatment received. Excess comorbidities have been shown to contribute to the lower curative treatment rates and poorer cancer survival among Indigenous Australians. In this study, the analysis showed that among cases without comorbidity, being Indigenous was associated with not receiving any cancer treatment. This study finding suggests that factors other than, or in conjunction with, comorbidity status may play a role (Moore et al. 2014).
The study also noted of particular concern are the reasons why treatment was not received by Indigenous Australians without comorbidities, who lived in an urban setting where cancer services are accessible, were not socially disadvantaged, and had localised cancer at diagnosis. The study suggested that understanding of reasons for treatment disparities in this group may enable cancer care providers to improve treatment uptake and survival. The study found that reasons for not receiving treatment were not routinely documented and recommended that the views of patients and health services staff are sought so that barriers to treatment can be understood. The study also showed, similar to other reports, that irrespective of remoteness or socioeconomic status , Indigenous Australians received less treatment than non-Indigenous counterparts (Moore et al. 2014; Tervonen et al. 2016).
A small study explored Western Australian Aboriginal peoples’ perceptions, beliefs and understanding of cancer. The study found that misunderstanding, fear of death, fatalism, shame, preference for traditional healing, beliefs such as cancer is contagious and other spiritual issues affected their decisions around accessing services. The study suggested that these findings provide useful information for health providers who are involved in cancer-related service delivery (Shahid et al. 2009).
The CanDAD project underway in South Australia is an approach whereby Aboriginal communities are working with policy makers, service providers and researchers to change the way Indigenous cancer data are collected and analysed. It aims to develop an integrated comprehensive, cancer monitoring and surveillance system for Aboriginal people, while also incorporating their experiences with cancer services. It is likely to have relevance for other regions (Brown et al. 2016; Yerrell et al. 2016).
Indigenous status identification in cancer registry data is not consistent nationwide. A study of cancer registry data in New South Wales found many cases with missing Indigenous status. Once imputed, an additional 12–13% of Indigenous cancer cases were identified (Morrell et al. 2012).
One study of a cultural awareness training initiative for primary care health professionals in regional Victoria found that Aboriginal clients reported the difference that cultural training for BreastScreen staff had made and felt genuinely welcomed by clinic staff (Anderson 2012). Other studies reported similarly successful initiatives which resulted in increased numbers of Aboriginal women participating in breast screening programs (Jones et al. 2011).
A small qualitative study evaluated the acceptability of a cancer care team based at one New South Wales Aboriginal medical service in supporting patients’ cancer journeys and assessed improvements in access to cancer care. The evaluation found that the cancer care team provided a culturally safe and accessible service for clients. It showed improved accessibility of cancer care services, including the availability of home visits, transport and accompaniment to tertiary settings (Ivers et al. 2019). The evaluation was subsequently used to develop a pilot project and was used in an application for a Cancer Australia funded project to support Indigenous people with cancer (University of Wollongong 2021).
A systematic review conducted by Christie et al. in 2021 aimed to assess whether cultural safety affected breast cancer outcomes for Indigenous women in high income countries. Literature used in this review highlighted that the use of Indigenous methodologies and Indigenous researchers were effective when communicating with Indigenous women. This allowed Indigenous women to relate to the people talking about breast cancer, engaged them in seeking information about treatment options, and reduced anxiety around treatment processes. The review concluded that culture makes a real difference to Indigenous women when it comes to the breast cancer journey and highlights that women fared better when culture was incorporated into screening, diagnosis, treatment, and follow up care (Christie et al. 2021).
In 2016, an evaluation and outcomes framework was developed for the Victorian Cancer Survivorship Program Phase II grants scheme (VCSP2). The VCSP was established in 2011 to help develop innovative models of follow-up care and to address the needs of survivors following treatment. In its first phase (2011–14), the focus of the VCSP was on trialling collaborative models of care across acute, primary and community care sectors. Six pilot projects were funded and evaluated for effectiveness, acceptability, sustainability and transferability. From 2015, three of the pilot projects have been supporting a select number of cancer services across Victoria to implement their models of care through the VCSP2. The evaluation and outcomes framework was developed to inform the application of consistent evaluation measures and methods to the planning, conduct, delivery and evaluation of the VCSP2. While this framework was designed specifically for VCSP2, it may provide a useful guide to the development and implementation of evaluation activities in other jurisdictions or in cancer survivorship initiatives in Victoria (Coughlan 2016).
Implications
The rising death rates and widening of the gap for Indigenous Australians from cancer requires urgent action to implement a health system wide response. While some positive health effects of the recent reductions in smoking prevalence may be immediate and within the short term (such as in cardiovascular outcomes), there is a long lag before the changes will fully impact upon smoking-related cancer mortality. This means smoking-related cancer mortality may continue to rise over the next decade before reaching its peak (Lovett et al. 2017).
The lower survival rate for Indigenous Australians from some cancers may be partly explained by factors such as lower screening rates, later diagnosis, lower likelihood of receiving treatment, comorbidities and a greater likelihood of being diagnosed with cancers with poorer survival (Cunningham et al. 2008; Moore et al. 2014; Shahid et al. 2016; Supramaniam et al. 2011). A qualitative study on factors contributing to delayed diagnosis of cancer among Indigenous Australians identified multiple factors including contextual (socioeconomic deprivation), historical/political (impact of colonisation, racism), health system (reduced access to health services), and patient factors (shame, embarrassment, fear, psychological trauma, male stoicism) (Shahid et al. 2016).
The findings in this measure highlight the inequities in health system performance particularly with regard to cancer screening and treatment. Evidence suggests that improvements in cancer care for Indigenous Australians are required, including in cancer diagnosis, treatment and health support services so they are more accessible and acceptable to Indigenous Australians (Condon et al. 2014; Meiklejohn et al. 2016).
Factors such as miscommunication and social and cultural differences between patients and health care providers, poor understanding of medical advice, inherent racism in the health system, lack of transport, geographic isolation, and lack of Indigenous support persons, have already been cited as some of the reasons for the disparities in treatment outcomes for Indigenous Australians. Personalised cancer care, which addresses the clinical, social and overall health requirements of Indigenous patients, may improve cancer outcomes. This may be particularly important during the first year after diagnosis (Moore et al. 2014).
An understanding of Indigenous Australians’ beliefs and perceptions of cancer and their care-seeking behaviour is needed when planning and delivering more effective culturally safe interventions, screening and models of care. Cultural security, removing system barriers and technical and scientific excellence are all essential to ensure Indigenous Australians access culturally safe health services for earlier diagnosis and timely treatment (Shahid et al. 2009; Shahid et al. 2016).
A significant body of work over the past two decades has sought to raise awareness and embed concepts of cultural respect in the Australian health system which are fundamental to improving access to quality and effective health care and improve health outcomes for Indigenous Australians. There has been a longstanding commitment by Australian governments to enable this. The Cultural Respect Framework 2016–2026 plays a key role in reaffirming this commitment and provides a nationally consistent approach (AHMAC 2016). The Aboriginal and Torres Strait Islander Health Performance Framework plays a role in monitoring this commitment across several measures (see measure 3.08 Cultural competency). Monitoring is also supported by the Cultural safety in health care for Indigenous Australians: monitoring framework which covers three domains: how health-care services are provided, Indigenous patients’ experience of health care, and measures regarding access to health care (AIHW 2022b). The 2022 Cultural safety report showed that a commitment to achieving culturally safe health care by Indigenous-specific health care organisations was 95% in 2017-18, an increase from 86% in 2012-13, while noting the lack of data available for reporting on the policies and practices of mainstream health services (AIHW 2022b).
Quality data are critical to understanding the variations in cancer care and outcomes for Indigenous Australians. However, as reported in the literature, there is limited or incomplete data available on Indigenous Australians diagnosed with cancer (Cancer Australia 2015; Garvey et al. 2011; Jane et al. 2020; Yerrell et al. 2016). Inconsistent Indigenous status identification in cancer notifications in several jurisdictions has been a problem (AIHW 2013), and there is a need for primary health care services in particular to address under‑identification (Haigh et al. 2018; Jane et al. 2020). However, nationally, there is indication that accuracy in Indigenous status identification is improving (AIHW 2019).
The National Aboriginal and Torres Strait Islander Cancer Framework (the Framework) released in 2015 aims to address disparities and improve cancer outcomes for Indigenous Australians by ensuring timely access to good quality and appropriate cancer related services across the cancer continuum. It provides strategic direction by setting out seven priority areas for action and suggests enablers to help in planning. The priority areas include improving knowledge and attitudes about cancer; focusing on prevention activities; increasing participation in screening and immunisation; ensuring early diagnosis; delivering optimal and culturally appropriate treatment and care; involving, informing and supporting families and carers; and strengthening the capacity of cancer-related services to meet the needs of Indigenous Australians (Cancer Australia 2015).
The Framework also highlights the need for improved Indigenous identification, including in pathology requests and reports. It also suggests the need for routine national data collection, access and data linkage to allow national monitoring and reporting (Cancer Australia 2015).
The Health Plan is the overarching policy framework to drive progress against the Closing the Gap health targets and priority reforms. Implementation of the Health Plan aims to drive structural reform towards models of care that are prevention and early intervention focused, with greater integration of care systems and pathways across primary, secondary and tertiary care. The Health Plan includes Priority 5 Early intervention to provide accessible, timely, high quality, effective and culturally safe and responsive care. This includes an objective to deliver targeted action to improve cancer screening rates and care pathways for treatment. The National Aboriginal and Torres Strait Islander Cancer Framework and the Optimal Care Pathway (OCP) for Aboriginal and Torres Strait Islander people with cancer must also continue to be implemented to drive access to culturally safe and responsive cancer treatment and care, including by addressing barriers to identifying, treating and managing cancer. The role of Aboriginal Community Controlled Health Services is crucial in providing culturally safe and comprehensive primary care including in the prevention, screening and management of cancer care, which supports clients through the cancer care continuum and partners with other cancer care providers.
The Health Plan suggests that efforts should be targeted at providing strengths based, culturally safe and holistic, affordable services to ensure early intervention across the life course. Vital to manage the development or progression of health conditions over time, early intervention must focus on the conditions with the potential to become serious, but that are preventable and/or easily treatable. Early intervention priorities may differ between communities depending on their location. Therefore, place-based approaches must be locally determined and embed multidisciplinary care and partnerships. They must include pathways through primary health care (including identification of symptoms, diagnosis, treatment and follow-up care) to allied, specialist and tertiary care.
As part of the National Agreement on Closing the Gap, the health sector was identified as one of four initial sectors for joint national strengthening effort and the development of a three-year Sector Strengthening Plan. The Health Sector Strengthening Plan (Health-SSP) was developed in 2021, to acknowledge and respond to the scope of key challenges for the sector, providing 17 transformative sector strengthening actions. Developed in partnership with Aboriginal and Torres Strait Islander community-controlled health sector and other Aboriginal and Torres Strait Islander health organisations, the Health-SSP will be used to prioritise, partner and negotiate beneficial sector-strengthening strategies.
The policy context is at Policies and strategies.
References
-
AHMAC (Australian Health Ministers' Advisory Council) 2016. Cultural Respect Framework 2016-2026 for Aboriginal and Torres Strait Islander health. Canberra: AHMAC.
-
AIHW (Australian Institute of Health and Welfare) 2013. Towards better Indigenous health data. Vol. Cat. no. IHW 93. Canberra: AIHW.
- AIHW 2018. Cancer in Aboriginal & Torres Strait Islander people of Australia. Canberra: AIHW.
- AIHW 2019. Cancer in Australia 2019. Canberra: AIHW.
- AIHW 2021. Cancer in Australia 2021. Canberra: AIHW.
-
AIHW 2022a. Australian Burden of Disease Study: Impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018. Canberra: AIHW.
-
AIHW 2022b. Cultural safety in health care for Indigenous Australians: monitoring framework. Canberra. Viewed 29/10/2022.
- AIHW & Cancer Australia 2013. Cancer in Aboriginal and Torres Strait Islander peoples of Australia: an overview. Canberra: AIHW.
- Banham D, Roder D & Brown A 2018. Comorbidities contribute to the risk of cancer death among aboriginal and non-aboriginal south Australians: analysis of a matched cohort study. Cancer Epidemiology 52:75-82.
- Banham D, Roder D, Eckert M, Howard NJ, Canuto K & Brown A 2019. Cancer treatment and the risk of cancer death among Aboriginal and non-Aboriginal South Australians: analysis of a matched cohort study. BMC health services research 19:771.
- Breast Cancer Network Australia 2018. Breast Cancer Network Australia's state of the nation report. Camberwell, Vic.
- Brown A, Roder D, Yerrell P, Cargo M, Reilly R, Banham D et al. 2016. Cancer Data and Aboriginal Disparities Project (CanDAD) – an overdue cancer control initiative. European Journal of Cancer Care 25:208-13.
- Cancer Australia 2015. National Aboriginal and Torres Strait Islander Cancer Framework 2015. Surry Hills, NSW: Cancer Australia.
-
Christie V, Green D, Amin J, Pyke C, Littlejohn K, Skinner J et al. 2021. What is the Evidence Globally for Culturally Safe Strategies to Improve Breast Cancer Outcomes for Indigenous Women in High Income Countries? A systematic Review. International Journal of Environmental Research and Public Health 18:6073.
-
Condon J, Garvey G, Whop L, Valery P, Thomas D, Gruen R et al. 2013. Aboriginal and Torres Strait Islander Australians and Cancer.
- Condon J, Zhang X, Baade P, Griffiths K, Cunningham J, Roder D et al. 2014. Cancer survival for Aboriginal and Torres Strait Islander Australians: a national study of survival rates and excess mortality. Population Health Metrics 12:1.
- Coughlan A 2016. The Development of an evaluation and outcomes framework for the Victorian Cancer Survivorship Program. (ed., Department of Health and Human Services). Melbourne: Victorian Government.
- Cramb SM 2012. The first year counts: cancer survival among Indigenous and non-Indigenous Queenslanders, 1997–2006. The Medical Journal of Australia 196:270-4.
- Cunningham J, Rumbold AR, Zhang X & Condon J 2008. Incidence, aetiology, and outcomes of cancer in Indigenous peoples in Australia. Lancet Oncology 9:585-95.
-
Dasgupta P, Martinez Harris V, Garvey G, Aitken J & Baade P 2022. Factors associated with cancer survival disparities among Aboriginal and Torres Strait Islander peoples compared with other Australians: A systematic review. Frontiers in Oncology 12.
- Garvey G, Cunningham J, Valery P, Condon J, Roder D, Bailie R et al. 2011. Reducing the burden of cancer for Aboriginal and Torres Strait Islander Australians: time for a coordinated, collaborative, priority-driven, Indigenous-led research program. Medical Journal of Australia 194:530-1.
- Haigh M, Burns J, Potter C, Elwell M, Hollows M, Mundy J et al. 2018. Review of cancer among Aboriginal and Torres Strait Islander people. Australian Indigenous HealthBulletin 18.
- Hall SE, Bulsara CE, Bulsara MK, Leahy TG, Culbong MR, Hendrie D et al. 2004. Treatment patterns for cancer in Western Australia: does being Indigenous make a difference? The Medical Journal of Australia 181:191-4.
- Harvey J, Budd A, Tanevska B, Ng F & Meere D 2018. Cervical screening in Australia 2018. Canberra: Australian Institute of Health and Welfare.
- Ivers R, Jackson B, Levett T, Wallace K & Winch S 2019. Home to health care to hospital: Evaluation of a cancer care team based in Australian Aboriginal primary care. Australian Journal of Rural Health 27:88-92.
- Jane B, Drew N, Elwell M, FitzGerald V, Hoareau J, Potter C et al. 2020. Overview of Aboriginal and Torres Strait Islander health status 2019.
- Li M, Roder D & McDermott R 2018. Diabetes and smoking as predictors of cancer in Indigenous adults from rural and remote communities of North Queensland–A 15‐year follow up study. International journal of cancer 143:1054-61.
- Lovett R, Thurber K & Maddox R 2017. The Aboriginal and Torres Strait Islander smoking epidemic: what stage are we at, and what does it mean? Public Health Research & Practice 27:e2741733.
- Meiklejohn JA, Adams J, Valery P, Walpole E, Martin J, Williams H et al. 2016. Health professional's perspectives of the barriers and enablers to cancer care for Indigenous Australians. European Journal of Cancer Care 25:254-61.
- Moore SP, Green AC, Bray F, Garvey G, Coory M, Martin J et al. 2014. Survival disparities in Australia: an analysis of patterns of care and comorbidities among indigenous and non-indigenous cancer patients. BMC Cancer 14:517.
- Morrell S, You H & Baker D 2012. Estimates of cancer incidence, mortality and survival in aboriginal people from NSW, Australia. BMC Cancer 12:168.
-
NACCHO (National Aboriginal Community Controlled Health Organisation) 2022. Bowel Cancer Screening. Viewed 29/10/2022.
- OECD (Organization for Economic Cooperation and Development) 2022. Deaths from cancer (indicator). Viewed 8/10/2022.
- Reath J & Carey M 2008. Breast and cervical cancer in Indigenous women: overcoming barriers to early detection. Australian Family Physician 37:178.
- Shahid S, Finn L, Bessarab D & Thompson S 2009. Understanding, beliefs and perspectives of Aboriginal people in Western Australia about cancer and its impact on access to cancer services. BMC health services research 9:132.
- Shahid S, Teng TK, Bessarab D, Aoun S, Baxi S & Thompson SC 2016. Factors contributing to delayed diagnosis of cancer among Aboriginal people in Australia: a qualitative study. BMJ Open 6.
- Supramaniam R, Gibberd A & O'Connell D 2011. Non-small cell lung cancer treatment and survival for Aboriginal people in NSW. Perth.
- Tapia KA, Garvey G, Mc Entee M, Rickard M & Brennan P 2017. Breast cancer in Australian Indigenous women: incidence, mortality, and risk factors. Asian Pacific journal of cancer prevention: APJCP 18:873.
- Tervonen HE, Aranda S, Roder D, Walton R, Baker D, You H et al. 2016. Differences in impact of Aboriginal and Torres Strait Islander status on cancer stage and survival by level of socio-economic disadvantage and remoteness of residence—A population-based cohort study in Australia. Cancer Epidemiology 41:132-8.
-
University of Wollongong 2021. Indigenous Health. Viewed 8/8/2022.
- Valery P, Coory M, Stirling J & Green AC 2006. Cancer diagnosis, treatment, and survival in Indigenous and non-Indigenous Australians: a matched cohort study. The Lancet 367:1842-8.
- Valery P, Youlden D, Baade P, Ward L, Green A & Aitken J 2013. Cancer survival in Indigenous and non-Indigenous Australian children: what is the difference? Cancer Causes & Control 24:2099-106.
- Yerrell PH, Roder D, Cargo M, Reilly R, Banham D, Micklem JM et al. 2016. Cancer data and Aboriginal disparities (CanDAD)—developing an advanced cancer data system for Aboriginal people in South Australia: a mixed methods research protocol. BMJ Open 6.