Key facts
Why is it important?
Environmental tobacco smoke, also known as second-hand smoke, is a significant cause of morbidity and mortality. The first evidence of harm to children from second-hand smoke (Colley 1974; Harlap & Davies 1974; Leeder et al. 1976) and increased lung cancer risk in adults (Hirayama 1981) emerged over 30 years ago. Global burden of disease analysis attributed 603,000 deaths to second-hand smoke in 2004 (Öberg et al. 2011).
There is consistent evidence that second-hand smoke causes lung cancer and ischaemic heart disease. It is also associated with an increased risk of respiratory diseases in adults, an increased risk of Sudden Infant Death Syndrome, and the exacerbation of asthma (Burke et al. 2012) and ear infections such as otitis media in children (Thomas & Stevens 2014) (see measure 1.15 Ear health). Second-hand smoke is associated with an increased risk of hospital readmission of Aboriginal and Torres Strait Islander infants with bronchitis and hospitalisation of Indigenous children for acute asthma (Giarola et al. 2014; McCallum et al. 2016). Exposure to second-hand smoke during pregnancy is also associated with an increased risk of obesity among offspring later in adolescence (Wang et al. 2014).
The home is a key setting for exposure to second-hand smoke for pregnant women and young children. Exposure to parents’ smoking in childhood is found to have pervasive vascular health effects into adulthood (Gall et al. 2014). Overcrowding in housing (see measure 2.02 Access to functional housing with utilities) increases the risk of such exposure and developing asthma. Smoking in cars is also a setting for child exposure to second-hand smoke (Agaku et al. 2014).
Data findings
Children’s exposure to environmental tobacco smoke is determined by whether the adults around them smoke, where they smoke (inside the house, outside the house or in the car) and how often they smoke.
Daily smoking
The 2018–19 National Aboriginal and Torres Strait Islander Health Survey (Health Survey) found that 455,400 (56%) Indigenous Australians reported they lived in households with daily smokers. Around 158,300 (57%) Indigenous children aged 0–14 lived in households with daily smokers and 9% (23,900) lived in households where people smoked inside the home (Table D2.03.9).
Smoking has declined significantly among Indigenous Australians aged 15 and over in recent years, from 47% in 2008 to 41% in 2018–19 (Table D2.15.1). This has contributed to a decline in the proportion of Indigenous children aged 0–14 living in households with daily smokers, from 65% to 57% over the same period (Table D2.03.7).
The 2014–15 National Aboriginal and Torres Strait Islander Social Survey found that Indigenous children aged 0–14 lived in households with a daily smoker at 2.7 times the rate for non-Indigenous children (57% compared with 21%, respectively) (Table D2.03.7). The 2018–19 Health Survey data on household smoking for Indigenous Australians was not comparable with non-Indigenous data from the National Health Survey 2017–18.
The proportion of Indigenous children aged 0–14 living in households with daily smokers was lowest in the Australian Capital Territory (39%) and highest in the Northern Territory (74%) (Table D2.03.3, Figure 2.03.1).
Figure 2.03.1: Proportion of Indigenous children aged 0–14 living in households with daily smoker(s), by jurisdiction, 2018–19
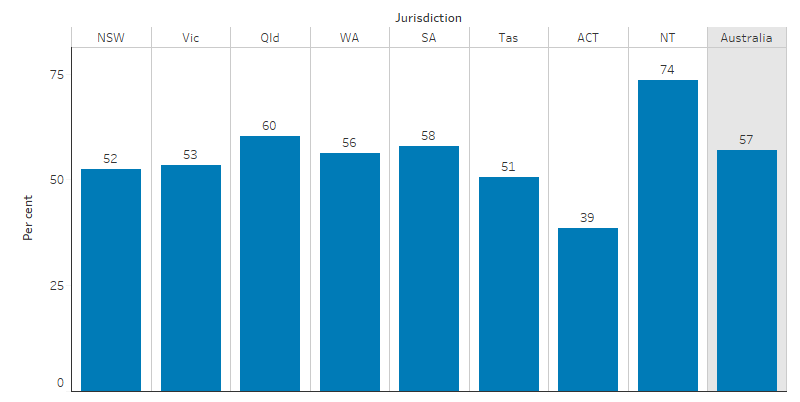
Source: Table D2.03.3. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Social Survey 2018–19.
In 2018–19, the proportion of Indigenous children aged 0–14 living with a daily smoker was 54% in Non-remote areas compared with 72% in Remote areas (Table D2.03.5, Figure 2.03.2).
Recent national-level declines in smoking among Indigenous adults have been driven by declines in Non-remote areas. In Remote areas, the proportion of Indigenous adults who smoke has not changed significantly for over a decade (Table D2.15.1). In Non-remote areas, the proportion of children living with daily smokers declined from 65% in 2004–05 to 54% in 2018–19, but in Remote areas, this had reduced by only 2 percentage points from 74% in 2004–05 to 72% in 2018–19 (Table D2.03.7, Figure 2.03.2).
Figure 2.03.2: Proportion of Indigenous children aged 0–14 living in households with daily smoker(s), by remoteness, 2004–05, 2008, 2012–13, 2014–15 and 2018–19
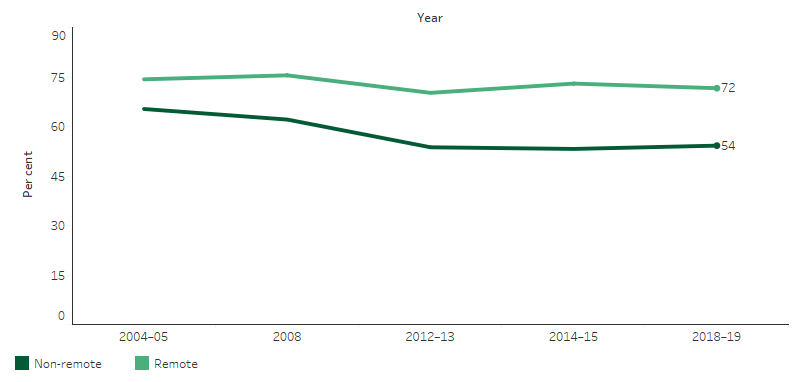
Source: Table D2.03.7. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Social Survey 2008, 2014–15; Australian Aboriginal and Torres Strait Islander Health Survey 2012–13; and National Aboriginal and Torres Strait Islander Health Survey 2004–05, 2018–19.
Smoking indoors
In 2018–19, 10% (83,900) of Indigenous Australians lived in households with a daily smoker who smoked indoors. Of Indigenous children aged 0–14, 9% (23,900) lived with someone who smoked indoors (Table D2.03.9, Figure 2.03.3).
Figure 2.03.3: Proportion of Indigenous Australians who lived in a household with a daily smoker and proportion who lived in a household where smoking occurred indoors, by age group, 2018–19
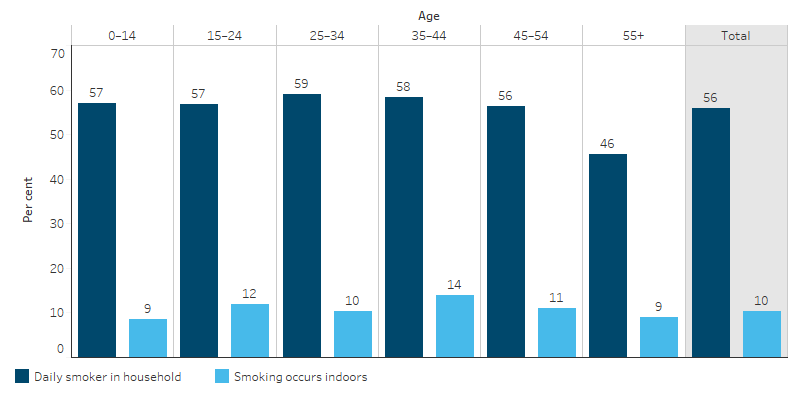
Source: Table D2.03.9. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
The proportion of Indigenous children aged 0–14 living in households where people smoked inside the home was highest in the Northern Territory (17%) (Table D2.03.4). The proportion of Indigenous children aged 0–14 living in households where people smoked inside was lower in Non-remote areas than Remote areas (8% compared with 12%) (Table D2.03.6).
Socioeconomic factors and exposure to tobacco smoke
Strong associations exist between the socioeconomic circumstances of Indigenous households and whether children are exposed to second-hand smoke. Indigenous children aged 0–14 living in lower-income households were 4 times as likely to live with a daily smoker as those living in households with the highest income (51% compared with 12%).
Among Indigenous children aged 0–14 living in rental housing, 17% were exposed to tobacco smoke indoors, compared with 7% of those living in homes that were owned or being purchased. Indigenous children living in households who had days without money for basic living expenses in the last 12 months were almost twice as likely to live in households where smoking occurred indoors than those who did not have days without money for basic living expenses (19% compared with 10%, respectively) (Table D2.03.8).
Research and evaluation findings
A recent review of international literature on interventions that aim to reduce children’s exposure to second-hand smoke found that further evidence is needed to determine the most effective ways of reducing exposure (Behbod et al. 2018).
Research has shown improvements in Indigenous Australians living in homes that are smoke-free and acceptance among Indigenous Australian smokers that homes and workplaces should be smoke-free. Smoke-free homes support successful smoking cessation (quit attempts and preventing relapse) along with a reduction in the consumption of cigarettes (see measure 2.15 Tobacco use). Qualitative research also suggests that smoke-free homes are associated with reductions in young people taking up smoking (Thomas et al. 2015; Thomas & Stevens 2014).
An evaluation of a family-centred intervention to reduce infant exposure to second-hand smoke among Indigenous families concluded that all household members (not only the mother) should cease smoking from the time of conception (Walker et al. 2015).
The results from an evaluation of an Indigenous-specific social marketing campaign ‘Give up Smokes for Good’ in South Australia indicated high awareness of the campaign among evaluation participants. Knowledge among the participants that smoking and second-hand smoke caused illness was high and around three-quarters of participants had imposed bans on smoking inside homes and cars. Culturally targeted awareness campaigns can be effective strategies for improving the awareness of second-hand smoke among Indigenous Australians (Maksimovic et al. 2015).
Reducing exposure to second-hand smoke through supporting smoke-free environments is one of five nationally consistent performance indicators for organisations receiving Tackling Indigenous Smoking program regional grant funding. The 2018 Tackling Indigenous Smoking Program Final Evaluation Report looked at how effective the program is, how well it meets the needs of Indigenous communities, and whether it is on target to achieve its long-term goals. The report found that the program is on track to achieve long-term objectives, which include the reduction of exposure to second-hand smoke and prevalence of smoking among Indigenous Australians (CIRCA 2019). It was also found that there was an increased focus on targeting health promotion for priority groups such as pregnant women and there was evidence indicating an increase in activity around smoke-free environments. There was an increase in smoke-free workplaces, with grant recipients reporting updating their workplace policies and supporting other workplaces to do the same. The report observed a notable increase in the number of smoke-free events and increased promotion of the benefits of smoke-free public spaces, homes and cars. Community members reported changes in second-hand smoke-related attitudes and behaviours, such as no longer smoking around children and delaying the smoking of a cigarette.
While the effects of smoking and second-hand smoke are well documented, in more recent years the concept of third-hand smoke has emerged as an area of research. Third-hand smoke refers to residual substances and chemicals from tobacco smoke that remain on or are absorbed by walls, furniture, clothes, toys and other objects and in dust after the tobacco has been smoked. These can be re-emitted into the air as gases over time. While these can produce toxic combinations of chemicals, it is not yet possible to fully understand the hazards to human health. However, in vitro and animal studies have demonstrated a range of health effects from third-hand smoke that are likely to be relevant for human health, including toxicity to the liver and lung, reduced wound healing and hyperactive behaviour (Campbell 2017).
Implications
The policy implications for addressing the dangers of second-hand smoke are similar to those for tobacco smoking in general (see measure 2.15 Tobacco use) and tobacco smoking during pregnancy (see measure 2.21 Health behaviours during pregnancy), and should be monitored in conjunction with these measures.
Further evaluation of interventions to encourage smoke-free homes, particularly in remote Indigenous Australian communities, will be important for future campaigns and policy development (Clough et al. 2018). Emerging evidence on the potential health effects of third-hand smoke may have implications for future approaches to environmental tobacco smoke exposure.
The policy context is at Policies and strategies.
References
- Agaku IT, Odukoya OO, Olufajo O, Filippidis FT & Vardavas CI 2014. Support for smoke-free cars when children are present: a secondary analysis of 164,819 U.S. adults in 2010/2011. European Journal of Pediatrics 173:1459-66.
- Behbod B, Sharma M, Baxi R, Roseby R & Webster P 2018. Family and carer smoking control programmes for reducing children's exposure to environmental tobacco smoke. Cochrane Database of Systematic Reviews:150.
- Burke H, Leonardi-Bee J, Hashim A, Pine-Abata H, Chen YL, Cook DG et al. 2012. Prenatal and Passive Smoke Exposure and Incidence of Asthma and Wheeze: Systematic Review and Meta-analysis. Pediatrics 129:735-44.
- Campbell MA, Ford, C., Winstanley, M.H., 2017. Tobacco in Australia: Facts and issues. Melbourne: Cancer Council Victoria.
- CIRCA (Cultural and Indigenous Research Centre Australia) 2019. Tackling Indigenous Smoking Program Final Evaluation Report, July 2018.
- Clough AR, Grant K, Robertson J, Wrigley M, Nichols N & Fitzgibbon T 2018. Interventions to encourage smoke-free homes in remote indigenous Australian communities: a study protocol to evaluate the effects of a community-inspired awareness-raising and motivational enhancement strategy. BMJ Open 8.
- Colley JR 1974. Respiratory symptoms in children and parental smoking and phlegm production. British Medical Journal 2:201-4.
- Gall S, Huynh QL, Magnussen CG, Juonala M, Viikari JS, Kahonen M et al. 2014. Exposure to parental smoking in childhood or adolescence is associated with increased carotid intima-media thickness in young adults: evidence from the Cardiovascular Risk in Young Finns study and the Childhood Determinants of Adult Health Study. European Heart Journal 35:2484-91.
- Giarola BF, McCallum GB, Bailey EJ, Morris PS, Maclennan C & Chang AB 2014. Retrospective review of 200 children hospitalised with acute asthma. Identification of intervention points: a single centre study. Journal of paediatrics and child health 50:286-90.
- Harlap S & Davies AM 1974. Infant admissions to hospital and maternal smoking. The Lancet 1:529-32.
- Hirayama T 1981. Non-smoking wives of heavy smokers have a higher risk of lung cancer: a study from Japan. British Medical Journal (Clinical Research Edition) 282:183-5.
- Leeder SR, Corkhill R, Irwig LM, Holland WW & Colley JR 1976. Influence of family factors on the incidence of lower respiratory illness during the first year of life. British Journal of Preventive & Social Medicine 30:203-12.
- Maksimovic L, Shen D, Bandick M, Ettridge K & Eckert M 2015. Evaluation of the pilot phase of the 'Give up smokes for good' social marketing campaign. Health Promotion Journal of Australia 26:16-23.
- McCallum GB, Chatfield MD, Morris PS & Chang AB 2016. Risk factors for adverse outcomes of Indigenous infants hospitalized with bronchiolitis. Pediatric Pulmonology 51:613-23.
- Öberg M, Jaakkola MS, Woodward A, Peruga A & Prüss-Ustün A 2011. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. The Lancet 377:139-46.
- Thomas DP, Panaretto KS, Stevens M, Bennet PT & Borland R 2015. Smoke-free homes and workplaces of a national sample of Aboriginal and Torres Strait Islander people. The Medical Journal of Australia 202:S33-8.
- Thomas DP & Stevens M 2014. Aboriginal and Torres Strait Islander smoke-free homes, 2002 to 2008. Australian & New Zealand Journal of Public Health 38:147-53.
- Walker N, Johnston V, Glover M, Bullen C, Trenholme A, Chang A et al. 2015. Effect of a Family-Centered, Secondhand Smoke Intervention to Reduce Respiratory Illness in Indigenous Infants in Australia and New Zealand: A Randomized Controlled Trial. Nicotine & Tobacco Research 17:48-57.
- Wang L, Mamudu HM, Alamian A, Anderson JL & Brooks B 2014. Independent and joint effects of prenatal maternal smoking and maternal exposure to second-hand smoke on the development of adolescent obesity: a longitudinal study. Journal of Paediatrics & Child Health 50:908-15.

