Key facts
Why is it important?
Chronic diseases are major causes of illness, disability and death among Aboriginal and Torres Strait Islander people (see measures 1.02 Top reasons for hospitalisation and 1.23 Leading causes of mortality). It has been estimated that chronic diseases are responsible for 70% of the health gap between Indigenous and non‑Indigenous Australians (AIHW 2016). This includes conditions such as cardiovascular diseases (19% of the gap); mental and substance use disorders (14%); cancer (9%); chronic kidney disease (CKD); diabetes; vision loss; hearing loss; and certain respiratory, musculoskeletal, neurological and congenital disorders.
The Novel Coronavirus disease (COVID-19) primarily manifests as an acute respiratory illness with interstitial and alveolar pneumonia, but can affect multiple organs such as kidney, heart, digestive tract, blood and the nervous system (Naicker et al. 2020). People at risk of experiencing more serious illness if infected with COVID-19 include people with chronic medical conditions, people with compromised immune systems, the elderly and Indigenous Australians (State of Victoria 2020).
Effective management of chronic disease can delay the progression of disease, decrease the need for high-cost interventions, improve quality of life, and increase life expectancy (see measure 3.05 Chronic disease management). The development of care plans is one way in which the client and primary health care (PHC) providers can ensure appropriate care is arranged and coordinated with the multiple health services necessary to deliver quality care and support to people with chronic diseases.
A care plan is a written action plan containing strategies for delivering care that address an individual’s specific needs, particularly patients with chronic conditions and/or complex care needs. A care plan can be used to record information about the patient’s condition, actions the patient needs to take and the various services required to achieve management goals for the patient. Development of a care plan can also help encourage the patient to take informed responsibility for their care, including actions to help achieve the treatment goals. A care plan may involve one health professional, usually a general practitioner (GP) or other PHC doctor, or it may be negotiated with several service providers (e.g. GP, nurse, Aboriginal Health Worker, allied health professionals, community services providers) in consultation with the patient.
GPs are encouraged to develop care plans through a number of items under the Medicare Benefits Schedule (MBS). In July 2005, Chronic Disease Management items were introduced specifically focused on patients with chronic or terminal conditions who will benefit from a structured approach to management of their care needs. These include an item related to the development of a GP Management Plan (GPMP), an item for a Team Care Arrangement (TCA) where planning involves a broader team, and items for where GPs contribute to care plans developed by another service provider or to a review of those plans.
Data findings
Medicare GPMP and TCA claims
In 2017–18, there were 78,478 GPMP claims and 68,012 TCA claims for MBS services for Indigenous Australians—a steady increase in uptake since these items were introduced in July 2005. In the period 2009–10 to 2017–18, the rate of services claimed by Indigenous Australians has increased by 88% for GPMPs (from 69 to 142 per 1,000) and increased by 106% for TCAs (from 55 to 125 per 1,000) (Table D3.05.1, Figure 3.18.1).
In 2017–18, the rate of MBS claims was higher for Indigenous than non-Indigenous Australians for both GPMP claims (142 and 100 per 1,000, respectively) and TCA claims (125 and 85 per 1,000 respectively). The higher rate for Indigenous Australians was particularly noticeable from 2009–10 (Table D3.05.1, Figure 3.18.1).
Figure 3.18.1: Age-standardised rates of GP management plans and Team care arrangements claimed through Medicare, by Indigenous status, 2005–06 to 2017–18
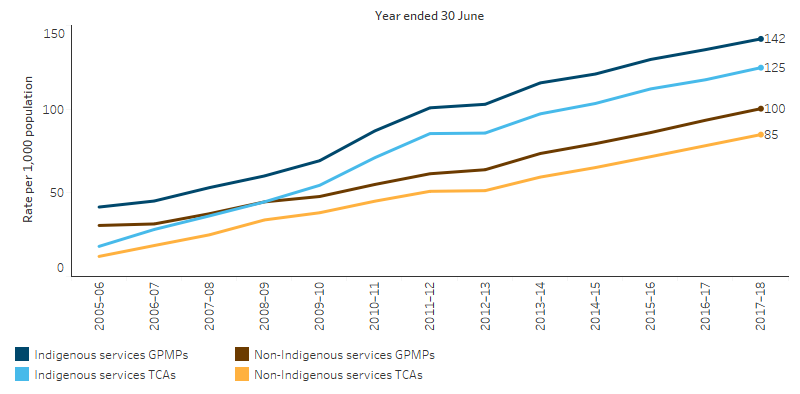
Source: Table D3.05.1. AIHW analysis of Medicare Data.
Over the period 2009–10 to 2017–18, the rate of MBS services claimed for a GPMP or TCA review for Indigenous Australians increased by 265%, from 60 to 215 per 1,000. MBS services claimed for the contribution of a GP to a multidisciplinary plan or review increased by 153% for Indigenous Australians over the same period (from 1.9 to 3.5 per 1,000 respectively), as did attendance by a GP to multidisciplinary case conferences (from 5 to 13 per 1,000 respectively) and attendance by a specialist to multidisciplinary case conferences (from 2.4 to 10.8 per 1,000 respectively) (Table D3.05.1, Figure 3.18.2).
Figure 3.18.2: Age-standardised rates of reviews and case conferences claimed through Medicare for Indigenous Australians, 2005–06 to 2017–18
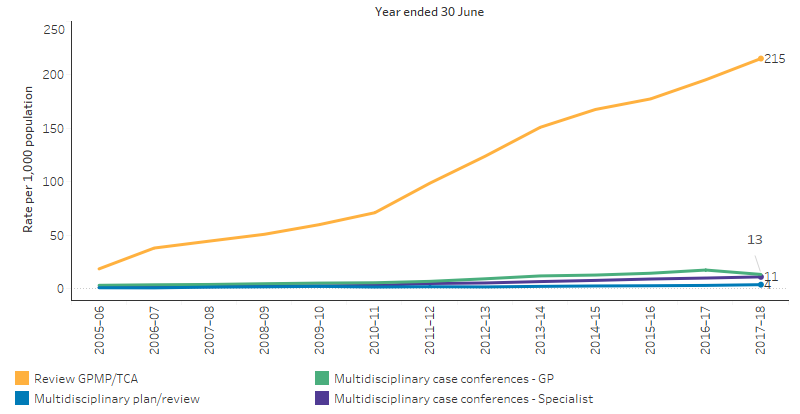
Source: Table D3.05.1. AIHW analysis of Medicare Data.
The higher rate of claims for Indigenous Australians for these MBS items than non‑Indigenous Australians is indicative that chronic diseases are responsible for 70% of the health gap between the two populations (AIHW 2016).
Primary health care organisations
Commonwealth-funded Indigenous primary health care (PHC) organisations provide national Key Performance Indicators (nKPI) data on a range of process of care measures related to chronic disease management.
As at December 2018, 43,740 regular (that is, has visited a particular PHC provider three or more times in the previous two years) Indigenous patients of PHC organisations had type 2 diabetes, and of these clients:
- 56% had a GPMP in the two years to December 2018, an increase of almost 3 percentage points from June 2017.
- 54% had a TCA in the two years to December 2018, an increase of 3 percentage points from June 2017 (Table D3.18.2, Table D3.05.16).
By remoteness, Major cities had the highest rate of Indigenous patients with a GPMP or a TCA while Very remote areas had the lowest (Figure 3.18.3). By jurisdiction Queensland had the highest rate of Indigenous patients with a GPMP or a TCA (Figure 3.18.4).
Figure 3.18.3: Proportion of Indigenous regular clients with type 2 diabetes who had a GPMP and TCA in the last 2 years, by remoteness area, Indigenous primary health-care organisations, June 2017 to December 2018
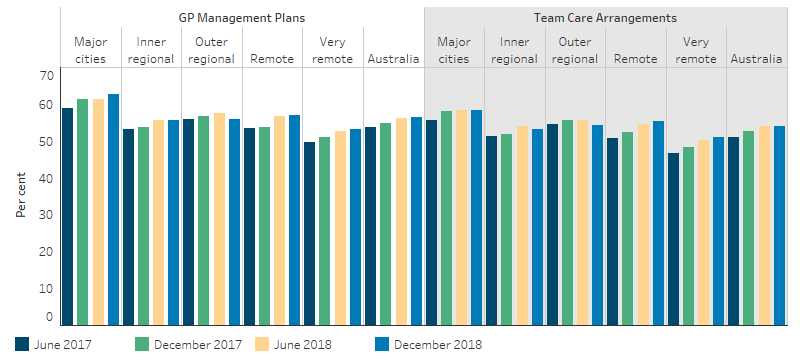
Source: Table D3.18.2. AIHW analysis of the National Key Performance Indicators for Aboriginal and Torres Strait Islander Primary Health Care collection.
Figure 3.18.4: Proportion of Indigenous regular clients with type 2 diabetes who had a GPMP and TCA in the last 2 years, by jurisdiction, Indigenous primary health-care organisations, June 2017 to December 2018
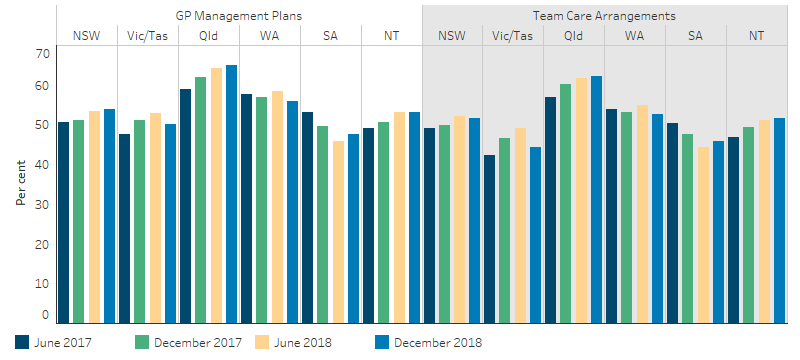
Source: Table D3.18.1. AIHW analysis of the National Key Performance Indicators for Aboriginal and Torres Strait Islander Primary Health Care collection.
In 2017–18, Commonwealth-funded Indigenous PHC organisations provided organisation-level data on chronic disease management to the Online Services Report data collection. All 198 Commonwealth-funded PHC organisations provided some form of care planning. This included:
- 99% kept track of clients needing follow-up appointments
- 100% used Patient Information Recall System, which automatically provide reminders for follow-up and routine health checks
- 88% established relationships with Aboriginal liaison officers at the local hospitals
- 72% shared care arrangements for chronic disease management
- 68% of staff regularly attended hospital/specialist appointments with clients
- 57% reported that discharge planning for Indigenous patients was well coordinated
- 55% of staff regularly visited clients in hospitals (Table D3.18.3).
Asthma management
Key elements of effective asthma management include a written asthma action plan and regular use of medications that control the disease and prevent exacerbations of the condition (AIHW 2011).
The 2018–19 National Aboriginal and Torres Strait Islander Health Survey showed that:
- 127,700 Indigenous Australians (16%) were living with asthma.
- after adjusting for differences in the age structure between the two populations, Indigenous Australians had asthma at 1.6 times the rate of non-Indigenous Australians (18% compared with 11%) (ABS 2019).
- 33% of Indigenous Australians with asthma who lived in Non-remote areas had a written asthma action plan, similar to the proportion of non-Indigenous Australians (32%).
- asthma action plans were most common among Indigenous children aged 0–14 (52%) (Figure 3.18.5).
- Indigenous Australians were more likely to go to hospital or an emergency department due to asthma compared with non-Indigenous Australians (16% and 7%, respectively) (Table D3.18.8).
Figure 3.18.5: Rate of people with asthma reporting having a written asthma action plan, by Indigenous status and age group, Non-remote areas, 2018–19
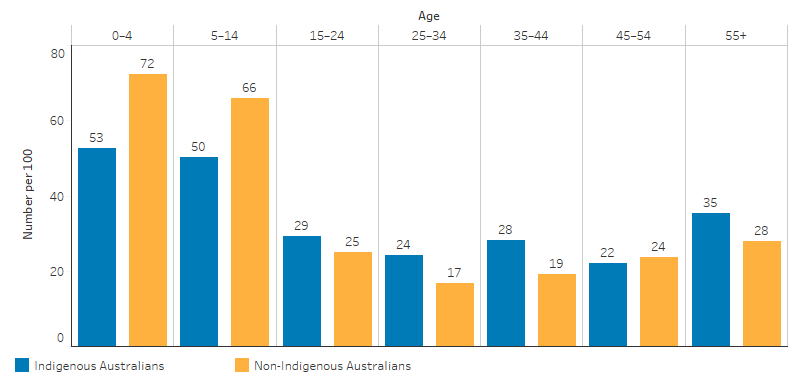
Source: Table D3.18.4. AIHW and ABS analysis of the National Aboriginal and Torres Strait Islander Health Survey 2018–19 and National Health Survey 2017–18.
Research and evaluation findings
As discussed in measure 3.05 Chronic disease management, the management of chronic disease in Indigenous PHC services has been demonstrated to result in improvement in various health outcomes (Bailie et al. 2007; Hoy et al. 2000; Hoy et al. 1999; McDermott et al. 2003; Rowley et al. 2000). It is therefore vital to work with clients and their families to support proactive management of chronic health conditions (Griew et al. 2007).
A study of general practice patients with type 2 diabetes found that, following implementation of care plans, the proportion of patients involved in multidisciplinary care, and the adherence to diabetes care guidelines increased. There were also improvements in patient metabolic control and cardiovascular risk factors (Zwar et al. 2007). Another study found an association between completing an annual cycle of care with good glycaemic control among diabetic patients (Esterman et al. 2016).
Aspin and others (2012) conducted a qualitative study and found that non-Indigenous health services struggled to meet the needs of Indigenous Australians with chronic illnesses (Aspin et al. 2012). Participants of the study identified poor access to culturally appropriate health services, dislocation from cultural support systems, exposure to racism, poor communication with health care professionals and economic hardship as negative influences. Negative experiences with specialists (for example. discrimination, feeling patronised, judged and blamed) have influenced participants’ decisions not to follow up on doctor referrals, with these having implications for continuity and coordination of care (Aspin et al. 2012).
However, participants pointed to cultural and traditional knowledge as well as insights from their own experiences as positive influences on their health and wellbeing (Aspin et al. 2012). Participants said that while they often felt overwhelmed and confused by the burden of chronic illness, they drew strength from being part of an Aboriginal community, having regular and ongoing access to primary health care, and being well-connected to a supportive family network. Within this context, elders played an important role in increasing people’s awareness of the impact of chronic illness on people and communities (Aspin et al. 2012).
A randomised controlled trial conducted between 2011 and 2013 found that participants with poorly controlled diabetes (HbA1c>8.5% or 69 mmol/mol) who received a chronic disease care plan and coordination saw a greater decrease in their HbA1c levels than the control group (who received the usual level of care) (McDermott et al. 2015; Schmidt et al. 2012). Over 18 months, there was a significant decrease in HbA1c results of 1% from baseline in the intervention group, from 10.8% (95 mmol/mol) to 9.8% (84 mmol/mol). The control group showed a smaller decrease of 0.2% from 10.6% (92 mmol/mol) to 10.3% (89 mmol/mol). (McDermott et al. 2015)
In 2016, Segal and others (2016) conducted an evaluation on the 2011–2013 diabetes randomised controlled trial mentioned above (McDermott et al. 2015; Schmidt et al. 2012). They found that while implementing a coordinated chronic disease care plan saw modest improvements in type 2 diabetes, the intervention comes at a relatively high cost (about $10,060 per person over the 18 months intervention period) (Segal et al. 2016). The intervention model as it currently stands is probably a poor investment. However, they noted improvements in cost-effectiveness can be made, such as having a higher caseload per Indigenous health worker or improving service integration. Segal and others (2016) also noted that a longer follow-up period than 18 months may have found greater reductions in the hospitalisation rate.
Using the 2014 Commonwealth Fund International Health Policy Survey of adults aged 55 years and over, Holdsworth and others (2019) found that 25% of Indigenous Australian respondents reported that the chronic disease plan they were receiving helped them ‘a lot’ to control and manage their condition (Holdsworth et al. 2019). This was lower than for non-Indigenous Australians, where 64% reported the plan had helped them ‘a lot’. Holdsworth and others (2019) suggested that cultural acceptability of chronic disease treatment planning may be lacking and efforts should be made to address the cultural needs of Indigenous Australians (Holdsworth et al. 2019; Liaw et al. 2011).
A number of reviews have found chronic disease interventions most likely to be effective include: engaging primary care services in self-management support through education and training for GPs and practice nurses, and including self-management support in care plans linked to multidisciplinary team support (Dennis et al. 2008; Kowanko et al. 2012). Chronic disease interventions with the strongest outcomes include those with culturally tailored interventions, community educators, individualised plans, feedback, and high-intensity interventions (at least 10 contact times) delivered over a long period (at least six months) (Glazier et al. 2006; McDermott et al. 2015).
Information on the reviews of chronic disease management programs such as the Integrated Care Team program, Practice Inventive Program—Indigenous Health Incentive, and other Primary Health Care programs, can be found in measure 3.05 Chronic disease management.
Implications
Programs and interventions targeted at improving chronic disease management can lead to positive health outcomes for Indigenous Australians. The strong improvements in the uptake of GPMPs and TCAs (and at higher rates than non-Indigenous Australians), is encouraging. However, the high burden of disease experienced by Indigenous Australians from chronic disease suggests that these improvements have not yet met the need for care in the community. Chronic disease care is often complex and requires careful management by patients and care providers. Care providers need to provide high quality clinical care and do so in culturally safe ways to assist Indigenous Australians achieve optimum outcomes.
For primary health care services to play an effective role in chronic disease management, key features include: transparent work-practice systems backed by written disease management guidelines and manuals; appropriate staffing and training policies; delineated roles for all practitioner types; dedicated chronic disease management staff; intensive follow-up by health professionals; established relationships with hospitals, specialists and allied health care workers; effective recall and reminder systems; connections with other services; taking a holistic and patient-centred approach; and community participation in quality improvement processes (Bodenheimer et al. 2002; Daws et al. 2014; Panaretto et al. 2014; Reilly et al. 2016; Sav et al. 2013; Stoneman et al. 2014; Wagner et al. 1996).
The holistic, culturally safe and patient-centred approaches used by Aboriginal Community Controlled Health Services (ACCHS) to deliver chronic disease care means they are well placed to meet the needs of their clients and assist them with the complex care requirements for chronic disease. The presence of Indigenous Australian health staff in ACCHSs has been a key enabler to deliver culturally safe and effective health services to Indigenous Australians. ACCHSs have also pioneered the adoption of continuous quality improvement practices for clinical care (such as the national Key Performance Indicators covered in this measure) from which mainstream services can learn.
Primary Health Networks have a role in improving timely access to coordinated and multidisciplinary care for eligible Indigenous Australians with chronic disease. This includes care coordination to support patients to navigate the health system so that they receive access to the care they need in clinically appropriate timeframes, and support for mainstream health services to provide culturally appropriate care to the Indigenous Australians who attend these services.
Further research on specific issues that Indigenous Australians face with chronic disease treatment plans would help identify areas for improvement to maximise the benefit of treatment plans and the management of chronic diseases for Indigenous Australians.
The policy context is at Policies and strategies.
References
- ABS (Australian Bureau of Statistics) 2019. National Aboriginal and Torres Strait Islander Health Survey, 2018–19. 4715.0. Canberra: ABS.
- AIHW (Australian Institute of Health and Welfare) 2011. Asthma in Australia 2011: with a focus chapter on chronic obstructive pulmonary disease. Cat. no. ACM 22. Canberra: AIHW.
- AIHW 2016. Australian Burden of Disease Study: Impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011. (ed., AIHW). Canberra.
- Aspin C, Brown N, Jowsey T, Yen L & Leeder S 2012. Strategic approaches to enhanced health service delivery for Aboriginal and Torres Strait Islander people with chronic illness: a qualitative study. BMC health services research 12:143.
- Bailie R, Si D, Dowden M & Lonergan K 2007. Audit and Best Practice for Chronic Disease: Project Final Report. Darwin: Menzies SHR.
- Bodenheimer T, Lorig K, Holman H & Grumbach K 2002. Patient self-management of chronic disease in primary care. JAMA 288:2469-75.
- Daws K, Punch A, Winters M, Posenelli S, Willis J, MacIsaac A et al. 2014. Implementing a working together model for Aboriginal patients with acute coronary syndrome: an Aboriginal Hospital Liaison Officer and a specialist cardiac nurse working together to improve hospital care. Australian Health Review 38:552-6.
- Dennis SM, Zwar N, Griffiths R, Roland M, Hasan I, Powell Davies G et al. 2008. Chronic disease management in primary care: from evidence to policy. The Medical Journal of Australia 188:S53-6.
- Esterman A, Fountaine T & McDermott R 2016. Are general practice characteristics predictors of good glycaemic control in patients with diabetes? A cross-sectional study. The Medical Journal of Australia 204:23.
- Glazier RH, Bajcar J, Kennie NR & Willson K 2006. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes care 29:1675-88.
- Griew R, Tilton E, Stewart J, Eades S, Lea T, Peltola C et al. 2007. Family Centred Primary Health Care: review of evidence and models (ed., Office of Aboriginal and Torres Strait Islander Health, Department of Health and Ageing). Canberra: OATSIH.
- Holdsworth S, Corscadden L, Levesque JF & Russell G 2019. Factors associated with successful chronic disease treatment plans for older Australians: Implications for rural and Indigenous Australians. Australian Journal of Rural Health 27:290-7.
- Hoy W, Baker P, Kelly A & Wang Z 2000. Reducing premature death and renal failure in Australian Aboriginals. The Medical Journal of Australia 172:473-8.
- Hoy W, Kelly A, Jacups S, McKendry K, Baker P, MacDonald S et al. 1999. Stemming the tide: reducing cardiovascular disease and renal failure in Australian Aborigines. Australian & New Zealand Journal of Medicine 29:480-3.
- Kowanko I, Helps Y, Harvey P, Battersby M, McCurry B, Carbine R et al. 2012. Chronic condition management strategies in Aboriginal communities: final report 2011. Adelaide: Flinders University, Aboriginal Health Council of South Australia.
- Liaw ST, Lau P, Pyett P, Furler J, Burchill M, Rowley K et al. 2011. Successful chronic disease care for Aboriginal Australians requires cultural competence. Australian and New Zealand journal of public health 35:238-48.
- McDermott R, Schmidt B, Preece C, Owens V, Taylor S, Li M et al. 2015. Community health workers improve diabetes care in remote Australian Indigenous communities: results of a pragmatic cluster randomized controlled trial. BMC health services research 15:1-8.
- McDermott R, Tulip F, Schmidt B & Sinha A 2003. Sustaining better diabetes care in remote Indigenous Australian communities. British Medical Journal 327:428.
- Naicker S, Yang C-W, Hwang S-J, Liu B-C, Chen J-H & Jha V 2020. The Novel Coronavirus 2019 epidemic and kidneys. Kidney International 97:824-8.
- Panaretto KS, Wenitong M, Button S & Ring IT 2014. Aboriginal community controlled health services: leading the way in primary care. The Medical Journal of Australia 200:649-52.
- Reilly R, Evans K, Gomersall J, Gorham G, Peters MDJ, Warren S et al. 2016. Effectiveness, cost effectiveness, acceptability and implementation barriers/enablers of chronic kidney disease management programs for Indigenous people in Australia, New Zealand and Canada: a systematic review of mixed evidence. BMC health services research 16:119.
- Rowley K, Gault A, McDermott R, Knight S, McLeay T & O'Dea K 2000. Reduced prevalence of impaired glucose tolerance and no change in prevalence of diabetes despite increasing BMI among Aboriginal people from a group of remote homeland communities. Diabetes care 23:898-904.
- Sav A, Kendall E, McMillan SS, Kelly F, Whitty JA, King MA et al. 2013. 'You say treatment, I say hard work': treatment burden among people with chronic illness and their carers in Australia. Health Soc Care Community 21:665-74.
- Schmidt B, Wenitong M, Esterman A, Hoy W, Segal L, Taylor S et al. 2012. Getting better at chronic care in remote communities: study protocol for a pragmatic cluster randomised controlled of community based management. BMC Public Health 12:1017.
- Segal L, Nguyen H, Schmidt B, Wenitong M & McDermott R 2016. Economic evaluation of Indigenous health worker management of poorly controlled type 2 diabetes in north Queensland. Medical Journal of Australia 204:196-.
- Stoneman A, Atkinson D, Davey MA & Marley JV 2014. Quality improvement in practice: improving diabetes care and patient outcomes in Aboriginal Community Controlled Health Services. BMC health services research 14:481.
- State of Victoria 2020. Coronavirus disease (COVID-19) Supplementary guidance for health services and general practitioners – Chronic disease management (ed., Department of Health and Human Services). Melbourne: Victorian Government.
- Wagner EH, Austin BT & Von Korff M 1996. Organizing care for patients with chronic illness. The Milbank Quarterly 74:511-44.
- Zwar NA, Hermiz O, Comino EJ, Shortus T, Burns J & Harris M 2007. Do multidisciplinary care plans result in better care for patients with type 2 diabetes? Australian Family Physician 36:85-9.

