Key facts
Why is it important?
Chronic diseases are long-lasting conditions with a persistent impact upon health and with social and economic consequences that can impact on peoples’ quality of life. Chronic diseases are the leading causes of illness, disability and death among Aboriginal and Torres Strait Islander people (see measures 1.02 Top reasons for hospitalisation and 1.23 Leading causes of mortality) and are estimated to be responsible for 70% of the health gap (AIHW 2016a). Effective management of chronic disease can delay the progression of disease, improve quality of life, increase life expectancy, and decrease the need for high-cost interventions leading to net savings (Thomas et al. 2014; Zhao et al. 2014). It is therefore a key factor in meeting the target of closing the life expectancy gap between Indigenous and non-Indigenous Australians within a generation.
For the purposes of Medicare, a chronic medical condition is one that has been (or is likely to be) present for six months or longer, for example, asthma, cancer, cardiovascular disease, diabetes, musculoskeletal conditions and stroke. There is no list of eligible conditions. However, the chronic disease management items in Medicare are designed for patients who require a structured approach, including those requiring ongoing care from a multidisciplinary team (DoH 2014). Specific items include General Practitioner Management Plans and Team Care Arrangements, which are used by doctors to plan and coordinate the care of patients who have chronic or terminal medical conditions. This recognises that good quality care for people with chronic disease often involves numerous health care providers across multiple settings and the engagement of the client and their family in self-management of the condition (NHPAC 2006).
The primary health care (PHC) provider plays a central role in the management of chronic disease and appropriate, affordable, acceptable and comprehensive primary health care is critical for improving the health of Indigenous populations worldwide (NHPAC 2006). The PHC provider: identifies patients with asymptomatic disease through systematic or opportunistic screening; develops a management plan with the patient and their family; regularly assesses the extent to which the chronic illness is controlled; conducts regular checks to identify early signs of complications; and issues referrals to specialist care as needed. Aboriginal Community Controlled Health Services (ACCHS) have a particularly important role in delivering culturally competent comprehensive health care for Indigenous Australians with chronic diseases. Chronic diseases are often complex, and patients often need assistance in managing their condition(s) and navigating the complex health system.
Data findings
Medicare Benefits Schedule
The Medicare Benefits Schedule (MBS) includes items for general practitioner management plans (GPMPs) and team care arrangements (TCAs) to support a structured approach to the management of patients with chronic or terminal conditions.
Between 2009–10 and 2017–18, the rate of MBS claims by Indigenous Australians for TCAs increased from 55 per 1,000 to 125 per 1,000, and was 1.5 times the rate for non-Indigenous Australians in 2017–18 (85 per 1,000), after adjusting for differences in age structure of the two populations. The rate of MBS claims for GPMPs was also higher for Indigenous than non-Indigenous Australians (1.4 times the rate, 142 and 100 per 1,000, respectively) (Table D3.05.1, Figure 3.05.1, Figure 3.05.2).
In 2017–18, for Indigenous Australians aged 15 and over, there were 70,197 MBS claims for the preparation of a GPMP; 61,666 for coordination of TCAs; 101,482 for multidisciplinary plans/reviews, 63,454 for practice nurse or Aboriginal Health Practitioner services; and 2,304 for follow up Aboriginal Health Worker Services for allied health items related to chronic disease (Table D3.05.2) (see measure 3.18 Care planning for chronic disease).
Figure 3.05.1: Age-standardised rates of selected GPMPs and TCAs claimed through Medicare by Indigenous status, 2005–06 to 2017–18
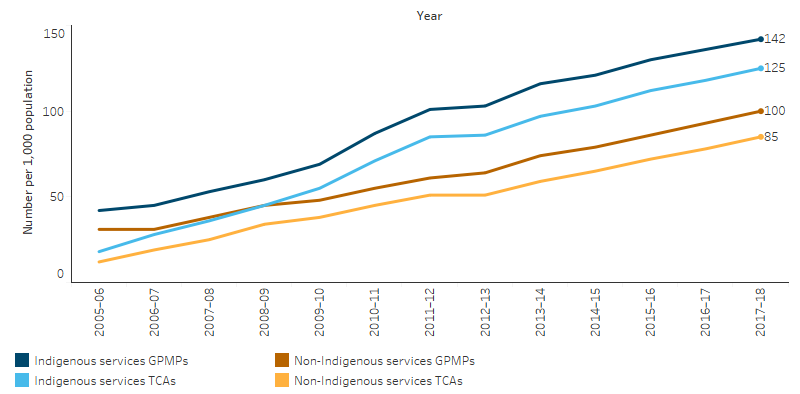
Source: Table D3.05.1. AIHW analysis of Medicare Data.
In 2017–18, there were 105,739 MBS services claimed for a GP review of GPMPs or the coordination of a TCA review for Indigenous patients. After adjusting for differences in age structure between the two populations, Indigenous Australians had a review for a GPMP or TCA at 1.7 times the rate for non-Indigenous Australians (215 per 1,000 compared with 129 per 1,000) (Table D3.05.1).
MBS claim rates for Indigenous patients accessing specialist providers (339,868) was almost half the rate of non-Indigenous patients (598 per 1,000 and 1,070 per 1,000, respectively). Allied health items were claimed at a rate of 480 per 1,000 for Indigenous patients (287,305 claims), slightly lower than the rate for non-Indigenous patients (505 per 1,000) (Table D3.14.23, Figure 3.05.2).
Figure 3.05.2: Age-standardised rate of selected MBS services claimed, by Indigenous status, 2017–18
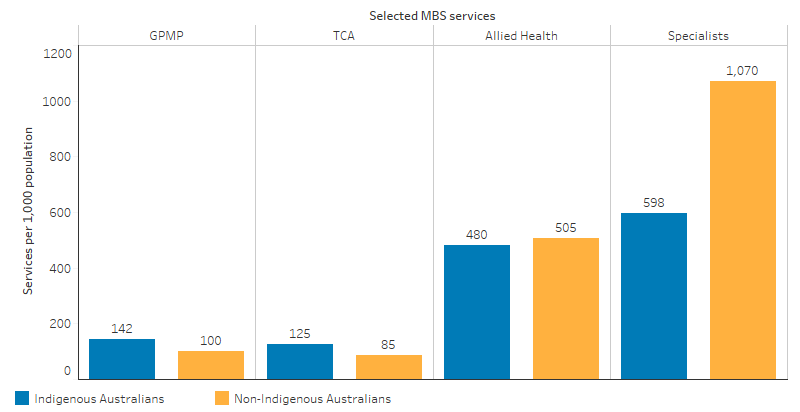
Source: Table D3.05.1, Table D3.14.23. AIHW analysis of Medicare Data.
Commonwealth-funded Indigenous-specific primary health care organisations
Commonwealth-funded Indigenous-specific primary health care organisations provide national Key Performance Indicators data on a range of process of care measures related to chronic disease management (AIHW 2019a). In December 2018, 43,740 regular clients of these organisations had type 2 diabetes. Of these clients, 56% had a GPMP in the two years to December 2018 and 54% had a TCA.
In the six months to December 2018, 49% of regular clients of Commonwealth-funded Indigenous-specific primary health care organisations with type 2 diabetes had an HbA1c test, with 38% reporting an HbA1c result in the recommended range. Sixty-five per cent had their blood pressure assessed, with 43% reporting a result in the recommended range. Sixty-three per cent had a kidney function test, with 81% reporting a result in the normal range (Table D3.05.16, Figure 3.05.3).
Figure 3.05.3: Tests and results for regular clients with type 2 diabetes, Commonwealth-funded Indigenous primary healthcare services, as at December 2018
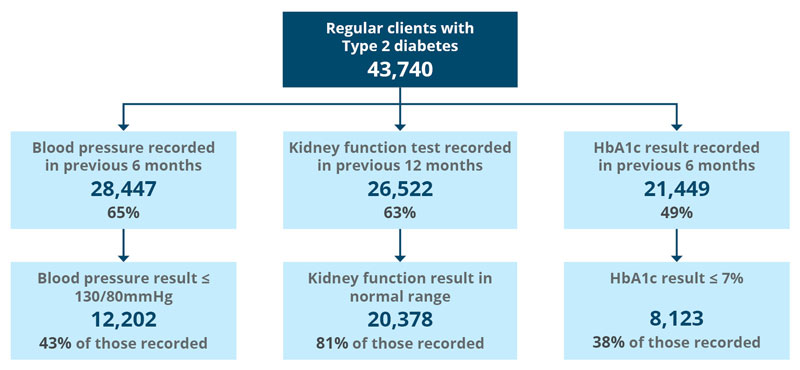
Source: Table D3.05.16. AIHW analysis of the National Key Performance Indicators for Aboriginal and Torres Strait Islander Primary Health Care collection.
In December 2018, of the 19,221 regular clients of Indigenous-specific primary health-care organisations with cardiovascular disease, 61% (11,701) had a kidney function test recorded. Of those with a kidney function test recorded, 77% (8,989) reported a result in the normal range (Table D3.05.16).
Indigenous-specific primary health care organisations also report on a range of services to manage chronic disease and provide continuity of care in the 2017–18 Online Services Report (AIHW 2019b). Of the 198 participating organisations:
- 171 (86%) employed a doctor,
- 195 (98%) kept track of clients needing follow-up,
- 174 (88%) had established relationships with Aboriginal liaison officers at the local hospitals,
- 143 (72%) had shared care arrangements for chronic disease management,
- 112 (57%) had well-coordinated discharge planning for Indigenous patients (for example, provision of medicines, transport arrangements, liaison with general practitioners and family) (Table D3.18.3, Table D3.19.6).
Findings from ABS survey data
In the 2018–19 National Aboriginal and Torres Strait Islander Health Survey, 64,400 Indigenous adults self-reported having diabetes or high blood sugar levels. Of those in Non-remote areas (46,720), 73% reported having a blood test (HbA1C) in the previous 12 months, similar to the rate for non-Indigenous adults (75%). Of those in all areas (Non-remote and Remote), foot checks had been completed for 77% of Indigenous adults responding compared with 74% for non-Indigenous adults. To manage their diabetes, 26% of Indigenous adults reported using insulin and 75% had taken lifestyle actions (diet, weight loss and exercise) (Table D3.05.13).
Of the 27,200 Indigenous adults who knew they had diabetes in 2012–13, 61% (16,600) had blood tests results indicating their diabetes was not well managed (compared with 44% for non-Indigenous Australians). This was more common for Indigenous males (72%) than females (53%) (ABS 2014).
Of Indigenous Australians who self-reported having circulatory conditions in 2018–19, 97% reported having had their blood pressure checked and 83% had their cholesterol checked in the previous 12 months, compared with 96% and 82%, respectively for non-Indigenous Australians (Table D3.05.14).
A recent study of Indigenous Australians in remote Northern Territory found that higher levels of primary care utilisation for renal disease reduced avoidable hospitalisations by 82–85%, deaths by 72–75%, and years of life lost (YLL) by 78–81%. For patients with ischaemic heart disease there was a reduction in avoidable hospitalisation of 63–78%, deaths 63–66% and years of life lost 69–73% (YLL) (Zhao et al. 2014).
Research and evaluation findings
Gomersall and others (2016) identified the importance of systematic reviews of primary health care research to inform chronic disease prevention and management (Gomersall et al. 2016). Better use of systematic reviews could include aligning review objectives with community-identified priorities, involving Indigenous community representatives as part of review teams, use of Indigenous cultural experts and ethical standards, and actions to ensure Indigenous Australians benefit from reviews.
Strategies for effective management of chronic disease should emphasise long-term, structured and well-organised approaches to chronic disease health care and research. Harvey and others (2013) (Harvey et al. 2013) noted the benefits of developing long-term working relationships with Indigenous communities. Results showed structured care planning and self-management strategies can improve health status and health outcomes for Indigenous Australians with chronic disease. Organised chronic disease management in primary health care services can lead to improved health outcomes (Esterman et al. 2016).
Care for Indigenous Australians with chronic disease involves both a variety of health providers as well as specific strategies for quality care delivery. Conway and others (2017) (Conway et al. 2017) explored the importance of self-management of chronic disease for populations with complex needs. The study identified the importance of good communication between patients and health providers and the value of Indigenous knowledge to support self-management strategies. Varying the delivery of health services is another strategy for quality care delivery. De Witt and others (2020) (de Witt et al. 2020) examined the role of flexible care delivery, such as telehealth, ‘Drop-in’ clinics, extension of primary health care clinic hours, longer patient consultations for Indigenous cancer patients and strategies to improve attendance such as appropriate cultural engagement with Indigenous clients. Ristevski and others (2020) (Ristevski et al. 2020) also found cultural connections and family to be vital for Indigenous cancer patient support. Roe and Kruske (2015) (Roe & Kruske 2015) found that family involvement in patient sessions resulted in improved communication with health care providers. Daws and others (2014) (Daws et al. 2014) found a “working together” model of care involving an Aboriginal Hospital Liaison Officer and a specialist cardiac nurse for Indigenous patients resulted in improved attendance at cardiac rehabilitation services.
Patient access to services is a key contributor to successful implementation of chronic disease care for Indigenous peoples (internationally) (Gibson et al. 2015). A 2014 study of chronic disease management in the Northern Territory (Thomas et al. 2014) found that even for people with the most complicated diabetes, regular attendance at their local health service for chronic disease checks reduced their risk of death significantly compared with those with newly diagnosed diabetes who rarely attended. The study concluded that improving access to primary care leads to better health outcomes for Indigenous Australian patients.
ACCHSs have a unique and irreplaceable function in chronic disease management for Indigenous Australians. Panaretto and others (2014) (Panaretto et al. 2014) argue that ACCHSs provide “superior performance to mainstream general practice” through using medical staff training, delivering best-practice care, and focussing on prevention, early intervention, comprehensive care and performance improvement relative to best-practice care indicators. The study also notes the importance of Aboriginal health workers at ACCHSs.
The supportive environment of an ACCHS is an ideal setting for culturally appropriate health care both face-to-face and via telehealth. This improves affordability and convenience, reduces patient stress and supports a holistic view of health. Aboriginal Health Workers play a key role in telehealth consultations by supporting Indigenous patients. In turn, patients experience less burden from travel and dislocation from community (Caffery et al. 2018).
Thomas and others (2014) analysed primary health care use by Indigenous Australians with diabetes in remote communities in the Northern Territory. They found that improved access to primary health care leads to health benefits to patients and cost savings to funding providers (Thomas et al. 2014). This is because more regular uptake of health care results in lower rates of hospitalisation and death, lower avoidable hospitalisations and fewer YLL. Gador-Whyte and others (2014) (Gador-Whyte et al. 2014) estimated the cost of treating patients with type 2 diabetes and chronic kidney disease at a remote ACCHS during 2009-10. While the service was relatively well funded compared with other Northern Territory primary care services, there was an estimated funding gap of around 44% of current operating costs. This would be required in order for the clinic to provide optimal treatment of each diabetes and chronic kidney disease patient. High staff turnover, acute care workload and low health literacy also hindered optimal chronic disease care.
The Australian Government Department of Health’s Integrated Team Care (ITC) Program is a combination of programs that originated as part of the Indigenous Chronic Disease Package – the Care Coordination and Supplementary Services Program and the Engaging Divisions of General Practice to Improve Indigenous Access to Mainstream Primary Care Program. Based on positive findings from the 2014 KPMG National Monitoring and Evaluation of the Indigenous Chronic Disease Package (KPMG 2014), funding for these programs was continued. The programs were amalgamated in 2016-17 to provide a comprehensive approach to support the management of chronic disease for Indigenous Australians.
The Department of Health reviewed Care Coordination in 2017 as part of the ITC Program. The review focused on the impact that access to coordinated and multidisciplinary care has had on improving health outcomes for Indigenous Australians with chronic health conditions. The review found that care coordination plays an integral role in improving access to services for Indigenous Australians with chronic conditions. Results of the ITC included improvements to: patient self-efficacy and self-management; adherence to treatment; health outcomes; trust between patient and health system; continuity of care; navigation of the health care system by patients; cultural appropriateness of mainstream primary care services; uptake of allied health, specialist and tertiary health care; and uptake of Indigenous-specific MBS items. There were also reduced barriers to accessing services and health aids (DoH 2018c).
The Department of Health also undertook a review of the Practice Incentives Program – Indigenous Health Incentive (PIP IHI) to examine its effectiveness in supporting ACCHSs and general practices to provide best practice chronic disease care for Indigenous Australians. As part of the review, a public consultation process sought stakeholder feedback to identify possible areas for improvement to the program. The public consultation process was finalised in July 2019. The Department of Health advised it was finalising the PIP IHI review with advice to the Australian Government to be provided in late 2019. A report detailing key insights gained through the consultation process is yet to be published.
In 2017, the Department of Health undertook two overarching evaluations of the Indigenous Australians’ Health Programme (IAHP) to assess the appropriateness and effectiveness of primary health care for Indigenous Australians and to inform implementation and refinement of the IAHP. The first is an evaluation of the Australian Government’s investment in Aboriginal and Torres Strait Islander Primary Health Care and has two phases. Phase One, Evaluation Co-design, was completed in mid-2018 with the development of a Monitoring and Evaluation Design Report (DoH 2018b). Phase Two, Evaluation Implementation, commenced in November 2018 and is being undertaken over a four-year period.
The second evaluation is an economic evaluation with two phases. Phase One focused on the return on investment of the IAHP and was completed in mid-2018 (DoH 2018a). The Phase One Report showed:
- Research literature provided evidence of a strong correlation between ACCHS episodes of care and prevented hospitalisations.
- The analysis of national data for this project found a preventative effect upon hospitalisations from ACCHS care.
- Provision of care through mainstream services is likely to be associated with worse health outcomes for Indigenous Australians because mainstream services provide a less comprehensive and less integrated approach.
- Indigenous Australians may face financial difficulties in accessing mainstream services, and if reliance were to be placed on mainstream services in lieu of ACCHSs, reduced attendance and adherence to treatment is highly likely due to services that may not meet their cultural needs and expectations.
Phase Two of the economic evaluation will evaluate the return on investment of the IAHP more broadly, starting with identifying and addressing data development needs for the evaluation. This will be undertaken as part of a broader evaluation of Aboriginal and Torres Strait Islander primary health care.
Implications
Programs and interventions targeted at improving chronic disease management can lead to positive health outcomes for Indigenous Australians. The strong improvements in the uptake of GPMP’s and TCA’s (and at higher rates than non-Indigenous Australians), is encouraging. However, the high burden of disease experienced by Indigenous Australians from chronic disease suggests that these improvements have not yet met the need for care in the community.
The disparity in MBS claims for specialists between Indigenous and non-Indigenous Australians is a consistent pattern and needs further exploration. This may in part reflect that not all services delivered by Indigenous primary health care (and some specialist services) can be claimed through Medicare. It may also reflect the higher proportions of Indigenous Australians compared to non-Indigenous Australians living in Remote areas, which affects access to specialists (AIHW 2016b).
A recent change was made to the MBS to assist with the difficulties in accessing dialysis treatment in Very remote areas. From 1 November 2018, registered nurses, Aboriginal Health workers, Aboriginal, and Torres Strait Islander health practitioners are able to use the MBS item 13105 for the supervision of dialysis in Very remote areas of Australia. This will provide greater access for patients, leading to better attendance for dialysis and improved health outcomes. This change will also help address the economic, cultural and social impacts on Indigenous Australian renal patients by providing greater access for these services on country.
Effective chronic disease care requires long-term strategies that promote and sustain engagement of Indigenous Australians with health services (see measure 3.08 Cultural competency). Strategies to support this include: flexible approaches that share decision-making and empower individuals to manage their conditions, strong local participation and connections with local communities, culturally appropriate education and health promotion, the availability of Aboriginal Health Workers, and raising awareness in communities through education and health promotion (Bailie C. et al. 2016; Bailie R.S. et al. 2004; Laycock & Brands 2015).
For primary health care services to play an effective role in chronic disease management, key features include: transparent work-practice systems backed by written disease management guidelines and manuals; appropriate staffing and training policies; delineated roles for all practitioner types; dedicated chronic disease management staff; intensive follow-up by health professionals; established relationships with hospitals, specialists and allied health care workers; effective recall and reminder systems; connections with other services; patient-centred approaches; and community participation in quality improvement processes (Bodenheimer et al. 2002; Daws et al. 2014; Panaretto et al. 2014; Reilly et al. 2016; Sav et al. 2013; Stoneman et al. 2014; Wagner et al. 1996).
The comprehensive, culturally competent and patient-centred approaches used by ACCHSs to deliver chronic disease care, means they are well placed to meet the needs of their clients and assist them with the complex care requirements for chronic disease. ACCHSs have also pioneered the adoption of continuous quality improvement practices (such as the national Key Performance Indicators covered in this measure) from which mainstream services can learn.
Primary Health Networks (PHNs) have a role in improving timely access to coordinated and multidisciplinary care for eligible Indigenous Australians with chronic disease. This includes care coordination to support patients to navigate the health system so that they receive access to the care they need in clinically appropriate timeframes, and support for mainstream health services to provide culturally competent care to the Indigenous Australians who attend these services.
The policy context is at Policies and strategies.
References
- ABS (Australian Bureau of Statistics) 2014. Australian Aboriginal and Torres Strait Islander Health Survey: Biomedical Results 2012–13. Canberra: ABS.
- AIHW (Australian Institute of Health and Welfare) 2016a. Australian Burden of Disease Study 2011: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011. Canberra: AIHW.
- AIHW 2016b. Australia's health 2016. Canberra: AIHW.
- AIHW 2019a. National Key Performance Indicators for Aboriginal and Torres Strait Islander primary health care: results to June 2018. Cat. no. IHW 211. Canberra: AIHW.
- AIHW 2019b. Aboriginal and Torres Strait Islander health organisations: Online Services Report—key results 2017–18. Aboriginal and Torres Strait Islander health services web report. Cat. no. IHW 212. . Canberra: AIHW.
- Bailie C, Matthews V, Bailie J, Burgess P, Copley K, Kennedy CM et al. 2016. Determinants and Gaps in Preventive Care Delivery for Indigenous Australians: A Cross-sectional Analysis. Frontiers in public health 4:34.
- Bailie RS, Si D, Robinson GW, Togni SJ & d'Abbs PH 2004. A multifaceted health-service intervention in remote Aboriginal communities: 3-year follow-up of the impact on diabetes care. The Medical Journal of Australia 181:195-200.
- Bodenheimer T, Lorig K, Holman H & Grumbach K 2002. Patient self-management of chronic disease in primary care. JAMA 288:2469-75.
- Caffery LJ, Bradford NK, Smith AC & Langbecker D 2018. How telehealth facilitates the provision of culturally appropriate healthcare for Indigenous Australians. Journal of telemedicine and telecare 24:676-82.
- Conway J, Tsourtos G & Lawn S 2017. The barriers and facilitators that indigenous health workers experience in their workplace and communities in providing self-management support: a multiple case study. BMC health services research 17:319.
- Daws K, Punch A, Winters M, Posenelli S, Willis J, MacIsaac A et al. 2014. Implementing a working together model for Aboriginal patients with acute coronary syndrome: an Aboriginal Hospital Liaison Officer and a specialist cardiac nurse working together to improve hospital care. Australian Health Review 38:552-6.
- de Witt A, Matthews V, Bailie R, Garvey G, Valery PC, Adams J et al. 2020. Communication, Collaboration and Care Coordination: The Three-Point Guide to Cancer Care Provision for Aboriginal and Torres Strait Islander Australians. International journal of integrated care 20:10-.
- DoH (Australian Government Department of Health) 2014. Chronic Disease Management (formerly Enhanced Primary Care or EPC) — GP services. Canberra: Australian Government Department of Health.
- DoH 2018a. Review of Care Coordination within the Integrated Team Care (ITC) Program – Summary report. Canberra: Australian Government Department of Health.
- DoH 2018b. Evaluation of the Australian Government’s Investment Aboriginal and Torres Strait Islander Primary Health Care through the Indigenous Australians’ Health Programme, Monitoring and Evaluation Design Report.
- DoH 2018c. Economic Evaluation of the Indigenous Australians’ Health Programme Phase 1 Report.
- Esterman AJ, Fountaine T & McDermott R 2016. Are general practice characteristics predictors of good glycaemic control in patients with diabetes? A cross-sectional study. The Medical Journal of Australia 204:23.
- Gador-Whyte AP, Wakerman J, Campbell D, Lenthall S, Struber J, Hope A et al. 2014. Cost of best-practice primary care management of chronic disease in a remote Aboriginal community. Medical Journal of Australia 200:663-6.
- Gibson O, Lisy K, Davy C, Aromataris E, Kite E, Lockwood C et al. 2015. Enablers and barriers to the implementation of primary health care interventions for Indigenous people with chronic diseases: a systematic review. Implementation science 10:71.
- Gomersall JS, Canuto K, Aromataris E, Braunack-Mayer A & Brown A 2016. Systematic review to inform prevention and management of chronic disease for Indigenous Australians: overview and priorities. Australian and New Zealand journal of public health 40:22-9.
- Harvey PW, Petkov J, Kowanko I, Helps Y & Battersby M 2013. Chronic condition management and self-management in Aboriginal communities in South Australia: outcomes of a longitudinal study. Australian Health Review 37:246-50.
- KPMG 2014. National Monitoring and Evaluation of the Indigenous Chronic Disease Package: Summary Report (2009-2013). (ed., Department of Health). Canberra: DoH.
- Laycock A & Brands J 2015. Chronic Illness Care for Aboriginal and Torres Strait Islander people: Final Report. Menzies SHR.
- NHPAC (National Health Priority Action Council) 2006. National Chronic Disease Strategy. (ed., Department of Health and Ageing). Canberra: DoHA.
- Panaretto KS, Wenitong M, Button S & Ring IT 2014. Aboriginal community controlled health services: leading the way in primary care. The Medical Journal of Australia 200:649-52.
- Reilly R, Evans K, Gomersall J, Gorham G, Peters MDJ, Warren S et al. 2016. Effectiveness, cost effectiveness, acceptability and implementation barriers/enablers of chronic kidney disease management programs for Indigenous people in Australia, New Zealand and Canada: a systematic review of mixed evidence. BMC health services research 16:119.
- Ristevski E, Thompson S, Kingaby S, Nightingale C & Iddawela M 2020. Understanding Aboriginal Peoples’ Cultural and Family Connections Can Help Inform the Development of Culturally Appropriate Cancer Survivorship Models of Care. JCO Global Oncology:124-32.
- Roe Y & Kruske S 2015. What indicators of Indigenous patient engagement can be identified in the patient record? A retrospective descriptive study. Australian Indigenous HealthBulletin 15:1-9.
- Sav A, Kendall E, McMillan SS, Kelly F, Whitty JA, King MA et al. 2013. 'You say treatment, I say hard work': treatment burden among people with chronic illness and their carers in Australia. Health Soc Care Community 21:665-74.
- Stoneman A, Atkinson D, Davey MA & Marley JV 2014. Quality improvement in practice: improving diabetes care and patient outcomes in Aboriginal Community Controlled Health Services. BMC health services research 14:481.
- Thomas S, Zhao Y, Guthridge SL & Wakerman J 2014. The cost‐effectiveness of primary care for Indigenous Australians with diabetes living in remote Northern Territory communities. Medical Journal of Australia 200:658-62.
- Wagner EH, Austin BT & Von Korff M 1996. Organizing care for patients with chronic illness. The Milbank Quarterly 74:511-44.
- Zhao Y, Thomas S, Guthridge SL & Wakerman J 2014. Better health outcomes at lower costs: the benefits of primary care utilisation for chronic disease management in remote Indigenous communities in Australia's Northern Territory. BMC health services research 14:463.

