Key facts
In 2018–19:
Why is it important?
Breastfeeding is recognised globally as the optimal method for feeding infants because it is linked to the child’s survival, growth and development (Victora et al. 2016). Breast milk is uniquely suited to the needs of newborns, providing nutrients that are readily absorbed by their digestive system and conferring both active and passive immunity for two years and beyond.
Australia’s infant feeding guidelines recommend exclusive breastfeeding of infants until around six months of age when solid foods are introduced and continued breastfeeding until the age of 12 months and beyond at the discretion of the mother and child. ‘Exclusive breastfeeding’ means that the infant receives only breast milk (including expressed milk) and medicines (including oral rehydration solutions, vitamins and minerals), but no infant formula or non-human milk (NHMRC 2013). For some Aboriginal and Torres Strait Islander infants living in poor housing conditions (see measure 2.02 Access to functional housing with utilities), breastfeeding offers additional protection where hygiene practices required for sterilising bottles may not be easily achieved or maintained.
Breastfeeding brings a range of health benefits for both the infant and the mother. It enhances bonding and attachment between the mother and the baby, reduces infant deaths and protects children against illnesses and conditions, including sudden infant death syndrome (SIDS), necrotising enterocolitis (NEC), diarrhoea, respiratory infections, otitis media, overweight or obesity, diabetes and childhood leukaemia. Breastfeeding also reduces the risk of hospitalisation for infants (Allen & Hector 2005; Duijts et al. 2009; Eidelman & Schanler 2012; Horta et al. 2015; Kramer et al. 2008). Maternal health benefits include a reduction in the incidence of breast and ovarian cancer and reduced maternal depression (Ji et al. 2018).
Data findings
The 2018–19 National Aboriginal and Torres Strait Islander Health Survey (Health Survey) showed that 85% of Indigenous children aged 0–3 years had been breastfed (Table D2.20.4).
There were comparable data for Indigenous and non-Indigenous children aged 0–2 years. In this age group, 87% of Indigenous children had previously been or were currently breastfed, compared with 93% of non‑Indigenous children (Table D2.20.5).
Indigenous children aged 0–2 were more likely than non‑Indigenous children to have been breastfed for at least one month to less than six months (30% compared with 19%). Indigenous children were less likely than non-Indigenous children to have been breastfed for 12 months or more (7% compared with 10%) (Table D2.20.5, Figure 2.20.1).
Figure 2.20.1: Breastfeeding duration for children aged 0–2 years, by Indigenous status, 2018–19
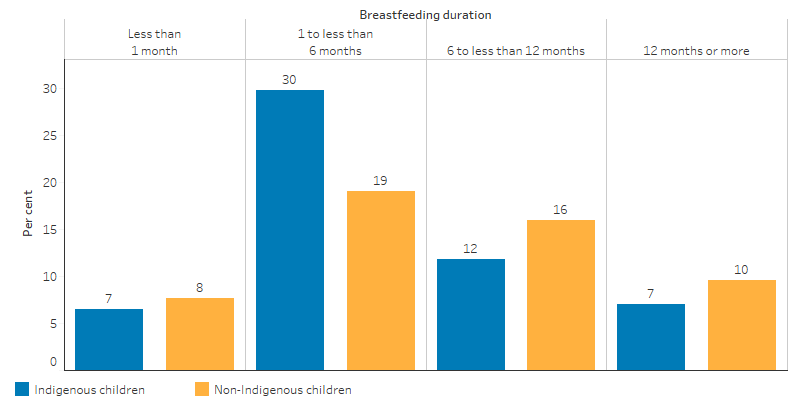
Source: Table D2.20.5. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19 and National Health Survey 2017–18.
The proportion of Indigenous children aged 0–2 years who had been breastfed ranged from 97% in Queensland to 64% in Victoria. In Victoria, the rate was significantly lower for Indigenous than for non-Indigenous children (64% compared with 92%), as was also the case in Tasmania (77% compared with 98%). Due to data quality issues, it is not possible to make comparisons in Western Australia, the Australian Capital Territory or the Northern Territory, but in all other jurisdictions the rate for Indigenous children was similar to the rate for non-Indigenous children (Table D2.20.6, Figure 2.20.2).
Figure 2.20.2: Proportion of children aged 0–2 years ever breastfed, by jurisdiction and Indigenous status, 2018–19
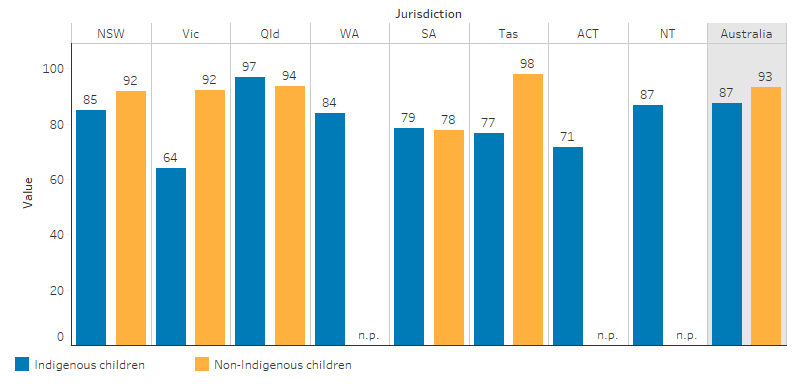
Source: Table D2.20.6. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19 and National Health Survey 2017–18.
The rate of breastfeeding is highest for Indigenous infants in Remote and Very remote areas (92%) and lowest for those in Major cities (84%) (Table D2.20.5, Figure 2.20.3).
Figure 2.20.3: Proportion of children aged 0–2 years ever breastfed, by remoteness and Indigenous status, 2018–19
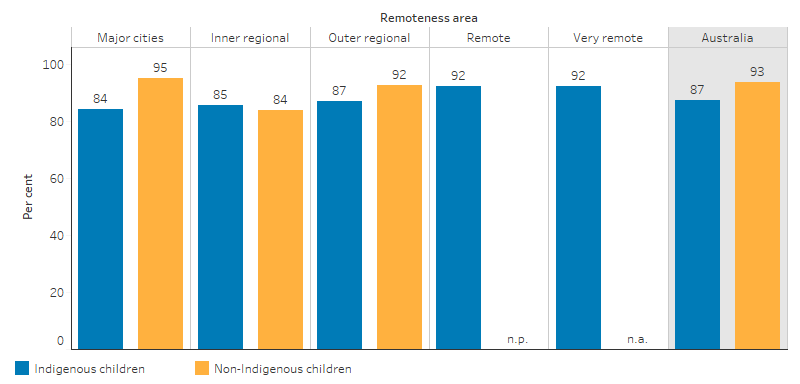
Source: Table D2.20.5. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19 and National Health Survey 2017–18.
Due to changes in how breastfeeding data items were recorded, outcomes in the 2018–19 Health Survey are not time series comparable with those from previous surveys. In past years, Indigenous breastfeeding rates ranged from as low as 76% in 2008 to as high as 83% in 2012–13. Across all survey years, breastfeeding rates were higher in Remote areas compared with Non-remote areas (Table D2.20.4, Figure 2.20.4).
Figure 2.20.4: Infants breastfed aged 0–3 years, by remoteness, Indigenous Australians, 2004–05, 2008, 2012–13 and 2014–15
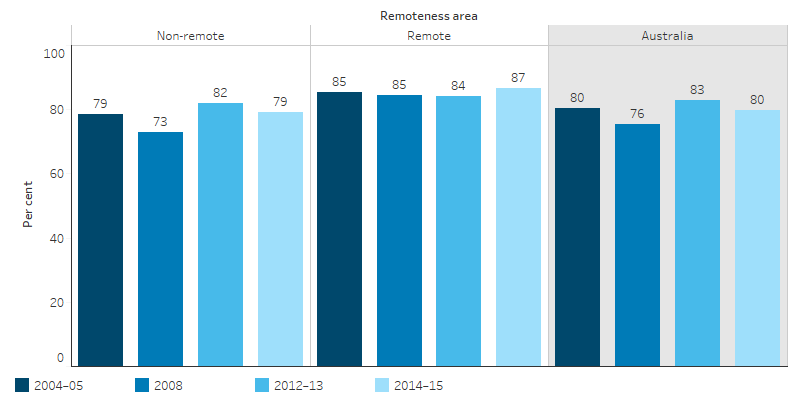
Source: Table D2.20.4. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2004–05; National Aboriginal and Torres Strait Islander Social Survey 2008, 2014–15; and Australian Aboriginal and Torres Strait Islander Health Survey 2012–13.
The 2010 Australian National Infant Feeding Survey found comparable rates of exclusive breastfeeding between the infants of Indigenous and non-Indigenous mothers in their first month (59% of Indigenous mothers and 61% of non‑Indigenous mothers). As infants increased in age the proportions of exclusive breastfeeding declined for both groups, but the decline for infants of Indigenous mothers was steeper than for infants of non‑Indigenous mothers. Due to data quality issues, the proportion of those exclusively breastfed to the recommended age of up to six months was not available, but for those aged up to five months only 11% of infants with Indigenous mothers were exclusively breastfed, compared with 27% of those with non-Indigenous mothers (AIHW 2011) (Figure 2.20.4). The Infant Feeding Survey found that almost half (45%) of infants of Indigenous mothers had received soft, semisolid or solid food by the age of four months, compared with 28% of infants of non-Indigenous mothers of the same age.
Figure 2.20.5: Proportion of infants exclusively breastfed to each month of age, by Indigenous status of mothers, 2010
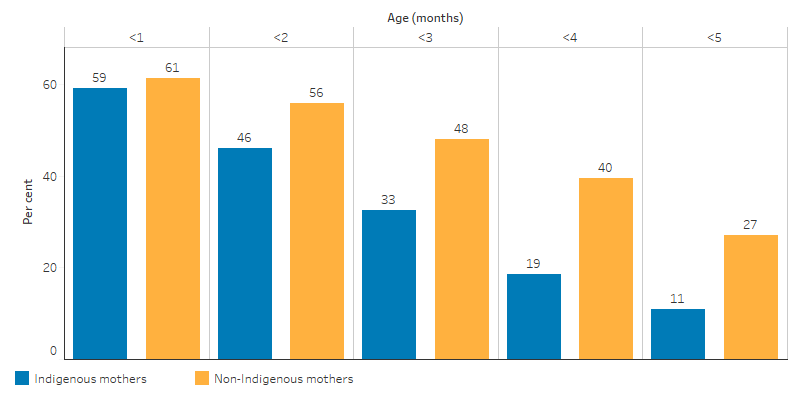
Source: AIHW 2011. 2010 Australian National Infant Feeding Survey: indicator results.
Reasons for ceasing breastfeeding
The 2012–13 Australian Aboriginal and Torres Strait Islander Health Survey indicated that for Indigenous infants, the main reason given for ceasing breastfeeding was ‘not producing any/adequate milk supply’ (24%), followed by ‘felt it was time’ (17%) and ‘baby not satisfied’ (15%) (ABS 2014). A non-Indigenous comparison is not available.
In 2018–19, 55% (36,390) of Indigenous children aged 0–3 years who had been breastfed were living with a current daily smoker and 4% (2,510) were living in a household where smoking occurred indoors (see measure 2.03 Environmental tobacco smoke) (Table D2.20.3).
Research and evaluation findings
Both maternal and family smoking is negatively associated with breastfeeding outcomes. Smoking affects the mother’s supply of milk, while exposure to passive smoking is a factor in reducing the duration of exclusive breastfeeding (Baheiraei et al. 2014; NHMRC 2013).
Research findings show a direct negative effect of maternal smoking on breastfeeding (Donath et al. 2004; Liu et al. 2006). Maternal smoking has been associated with reduced duration of breastfeeding (Amir 2001; Goldade et al. 2008) and also with maternal obesity (Amir & Donath 2007; Wojcicki 2011), maternal alcohol use (Dunn et al. 2006; Giglia 2010) and maternal depression (Dennis & McQueen 2007).
Excessive alcohol consumption, substance use or smoking during lactation potentially pose risks to the baby’s health and further research is needed to understand these relationships (Haastrup et al. 2014) (see 2.21 Health behaviours during pregnancy).
A small study in rural New South Wales found that Aboriginal women value trust and knowledge about infant feeding passed on to them from extended family members and women within their community (Helps & Barclay 2015). Another study in a Queensland urban area found that individual circumstances strongly influence infant feeding strategies and that community strengths are underused in supporting breastfeeding mothers (Foley et al. 2013).
There is also evidence of the effectiveness of culturally appropriate Indigenous health programs in Australia delivered within community-controlled holistic primary health care services. Multiple opportunities to provide mothers and communities with consistent breastfeeding promotion, education and support also occur when maternity care and maternal and child health services:
- follow a woman-centred, continuity of care model from pregnancy through to preschool age
- are delivered by Indigenous community-controlled organisations and Indigenous health professionals and other staff, including Indigenous health and childcare workers (COAG Health Council 2019).
Implications
Breastfeeding interventions for Indigenous Australians highlight the need to integrate culturally sensitive interaction and communication with programs to address multiple health and social issues that are barriers to optimal infant and young child feeding. However, there is a need for more research to be undertaken into the effectiveness of breastfeeding interventions for Indigenous populations in Australia and worldwide (Smith et al. 2018).
It is important that opportunities exist to promote breastfeeding in partnership with Indigenous Australian families and communities in educational settings and within the health sector, particularly in antenatal and postnatal care. Targeted breastfeeding programs and health promotion activities, including those aimed at reducing maternal and family smoking, can assist Indigenous Australian mothers and families in making informed, healthy choices.
The policy context is at Policies and strategies.
References
- ABS (Australian Bureau of Statistics) 2014. Microdata: Australian Aboriginal and Torres Strait Islander Health, Survey. Detailed Conditions and Other Health Data, 2012-13. Expanded Confidentialised Unit Record File, TableBuilder. Findings based on use of ABS Microdata. (ed., Australian Bureau of Statistics). Canberra: ABS.
- AIHW (Australian Institute of Health and Welfare) 2011. 2010 Australian National Infant Feeding Survey: indicator results. Cat. PHE 156. Canberra: AIHW
- Allen J & Hector D 2005. Benefits of breastfeeding. New South Wales Public Health Bulletin 16:42-6.
- Amir LH 2001. Maternal smoking and reduced duration of breastfeeding: a review of possible mechanisms. Early Human Development 64:45-67.
- Amir LH & Donath S 2007. A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC pregnancy and childbirth 7:9.
- Baheiraei A, Ghafoori F, Foroushani AR & Nedjat S 2014. The effects of maternal exposure to second-hand smoke on breast-feeding duration: A prospective cohort study. Journal of Public Health 22:13-22.
- COAG Health Council (Council of Australian Governments Health Council) 2019. The Australian National Breastfeeding Strategy: 2019 and Beyond. Canberra, .
- Dennis CL & McQueen K 2007. Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatrica 96:590-4.
- Donath S, Amir L & Team A 2004. The relationship between maternal smoking and breastfeeding duration after adjustment for maternal infant feeding intention. Acta Paediatrica 93:1514-8.
- Duijts L, Ramadhani MK & Moll HA 2009. Breastfeeding protects against infectious diseases during infancy in industrialized countries. A systematic review. Maternal & child nutrition 5:199-210.
- Dunn S, Davies B, McCleary L, Edwards N & Gaboury I 2006. The relationship between vulnerability factors and breastfeeding outcome. Journal of Obstetric, Gynecologic & Neonatal Nursing 35:87-97.
- Eidelman AI & Schanler RJ 2012. From the American academy of pediatrics: Policy statement, breastfeeding and the use of human milk: Section on breastfeeding. Pediatrics.
- Foley W, Schubert L & Denaro T 2013. Breastfeeding experiences of Aboriginal and Torres Strait Islander mothers in an urban setting in Brisbane. Breastfeeding Review 21:53.
- Giglia RC 2010. Alcohol and lactation: An updated systematic review. Nutrition & Dietetics 67:237-43.
- Goldade K, Nichter M, Nichter M, Adrian S, Tesler L & Muramoto M 2008. Breastfeeding and smoking among low‐income women: Results of a longitudinal qualitative study. Birth 35:230-40.
- Haastrup MB, Pottegård A & Damkier P 2014. Alcohol and breastfeeding. Basic & clinical pharmacology & toxicology 114:168-73.
- Helps C & Barclay L 2015. Aboriginal women in rural Australia; a small study of infant feeding behaviour. Women and Birth 28:129-36.
- Horta BL, Loret de Mola C & Victora CG 2015. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta-analysis. Acta Paediatrica 104:30-7.
- Ji H, Liu N, Yin Y, Wang X, Chen X, Li J et al. 2018. Oxytocin inhibits ovarian cancer metastasis by repressing the expression of MMP-2 and VEGF. Journal of Cancer 9:1379.
- Kramer MS, Aboud F, Mironova E, Vanilovich I, Platt RW, Matush L et al. 2008. Breastfeeding and child cognitive development: new evidence from a large randomized trial. Archives of general psychiatry 65:578-84.
- Liu J, Rosenberg K & Sandoval A 2006. Breastfeeding duration and perinatal cigarette smoking in a population-based cohort. American journal of public health 96:309-14.
- NHMRC (National Health and Medical Research Council) 2013. Infant Feeding Guidelines: Summary. (ed., Department of Health and Ageing). Canberra: NHMRC.
- Smith J, Cattaneo A, Iellamo A, Javanparast S, Atchan M, Gribble K et al. 2018. Review of effective strategies to promote breastfeeding.
- Victora CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J et al. 2016. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet 387:475-90.
- Wojcicki JM 2011. Maternal prepregnancy body mass index and initiation and duration of breastfeeding: a review of the literature. Journal of Women's Health 20:341-7.

